
Last update: 2/10/2017
Dual Eligible Special Needs Plans (D-SNP) 2017 Frequently Asked Questions (FAQs)
What is a FIDE SNP?
New Jersey has a Fully Integrated Dual Eligible Special Needs Plan (FIDE SNP) Program that is
available for individuals who have both Medicare and Medicaid benefits. A FIDE SNP is a special kind
of Medicare Advantage plan that combines all of the services offered by original Medicare and a
prescription drug plan, along with all of NJ FamilyCare’s managed care services.
Last year, each of the NJ Dual Eligible Special Needs Plans (D-SNPs) became FIDE SNPs when the
State added managed long-term services and supports (MLTSS) to the D-SNP benefit package. For
the purpose of this document, the terms “FIDE SNP” and “D-SNP” are used interchangeably.
When a member enrolls in a FIDE SNP, he or she will be automatically disenrolled from original
Medicare, their Part D prescription drug plan, and all of their Medicare and Medicaid benefits will be
covered by the FIDE SNP.
What FIDE SNP plans are available in my county?
• Please see the FIDE SNP options chart on page 3.
• Currently there are four FIDE SNP plans operating in the State of New Jersey. Please note that
these health plans have been approved in specific counties, so check the chart on page 3 to see
which counties are covered by specific FIDE SNP plans.
o You can contact your local State Health Insurance Assistance Program (SHIP) office at 1-800-
792-8820. They will help you select a FIDE SNP plan.
o Or you can contact Medicare at 1-800 MEDICARE (1-800-633-4227, TTY#: 1-877-486-2048),
24 hours a day, 7 days a week.
Search Online
At www.Medicare.gov, you will find a Medicare Plan Finder
that will let you know which
FIDE SNP plans are available
in your county.
Compare provider networks and drug lists!
https://www.medicare.gov/sig
n-up-change-plans/index.html
New!
As of January 1, 2017, a new FIDE SNP plan is available in New Jersey: Horizon NJ TotalCare (HMO
SNP). It will operate in 15 counties (please see the chart on page 3).
With the addition of Horizon NJ TotalCare, there will be a total of four health plans offering FIDE SNP,
and at least one FIDE SNP plan will be available in 20 of the state’s 21 counties (only Cape May county
will not have a FIDE SNP plan option in 2017).
Last update: 2/10/2017
FIDE SNP Program and Plan Features
All FIDE SNPs in New Jersey include extra features and benefits that go beyond traditional Medicare or
NJ FamilyCare plans, including:
•
Coverage of all Medicare and Medicaid benefits under a single plan, with a single member ID
card;
•
Plan benefits include, but are not limited to coverage for medical, dental, vision, hearing,
prescription drug, lab, podiatry, imaging, behavioral health and long-term services and supports;
•
A single provider network for each plan;
•
A single point of contact for each plan (Member Services);
•
$0 cost sharing for plan services and covered prescription drugs, as long as enrollees use
participating (in-network) providers (Cost sharing does not include patient pay liability for
assisted living or nursing facilities. Some members may have out of pocket costs for assisted
living or nursing facility.);
•
Behavioral health benefits under plan, including inpatient, outpatient, partial care, and certain
substance abuse services;
•
The same comprehensive dental plan as NJ FamilyCare Plan A;
•
Extra benefits not available from traditional Medicare or NJ FamilyCare; benefits differ from plan
to plan, but some examples include gym membership, Personal Emergency Response Systems
(which are otherwise only available to MLTSS members), and spending cards for over-the
counter health items;
•
All FIDE SNP members also have access to a dedicated Care Manager and Interdisciplinary
Care Team to assist in them in identifying and monitoring their health care needs, creating a
customized Plan of Care, and arranging necessary services. This is true even when a member
declines Care Management.
Things to keep in mind when joining a FIDE SNP:
•
Enrollees need to use participating (in-network) providers. Prospective members are
advised to check the online provider directory on the plan’s website or call the plan to determine
whether or not their current primary care providers, pharmacies, Durable Medical Equipment
(DME) providers, dentists, and other specialists are in the plan’s network. Please see the chart
on page 3 for links to FIDE SNP provider directories.
•
FIDE SNPs use formularies (approved drug lists). Prospective members should check the
plan’s online formulary or call the plan to determine whether or not their drugs are included in
the plan’s formulary. Please see the chart on page 3 for links to FIDE SNP web pages and
formulary look-ups.
•
Some plans may require referrals for certain services and specialist types. Be sure to ask
about the plan’s referral policy.
•
When enrolled in a FIDE SNP, all of an individual’s Medicare and Medicaid managed care
services, including MLTSS services (if clinically and financially eligible), will be covered
by that FIDE SNP. This includes Care Management.
•
Members who choose their current plan’s FIDE SNP may keep their MLTSS care manager
when switching over to the FIDE SNP option.
If I enroll in a FIDE SNP, will I have to choose a new primary care provider (PCP)?
Last update: 2/10/2017
A: All NJ FIDE SNPs require members to choose, or have chosen for them, a PCP who is in the FIDE
SNP network. Before enrolling in a new FIDE SNP, you should find out if your current PCP and other
preferred providers are in the FIDE SNP network.
What information will I receive once I enroll in the FIDE SNP?
A: Once enrolled, you will receive a welcome packet from your plan. That packet should include an ID
card, an Evidence of Coverage document, a Summary of Benefits and other helpful information
about provider networks, covered services and useful phone numbers and websites.
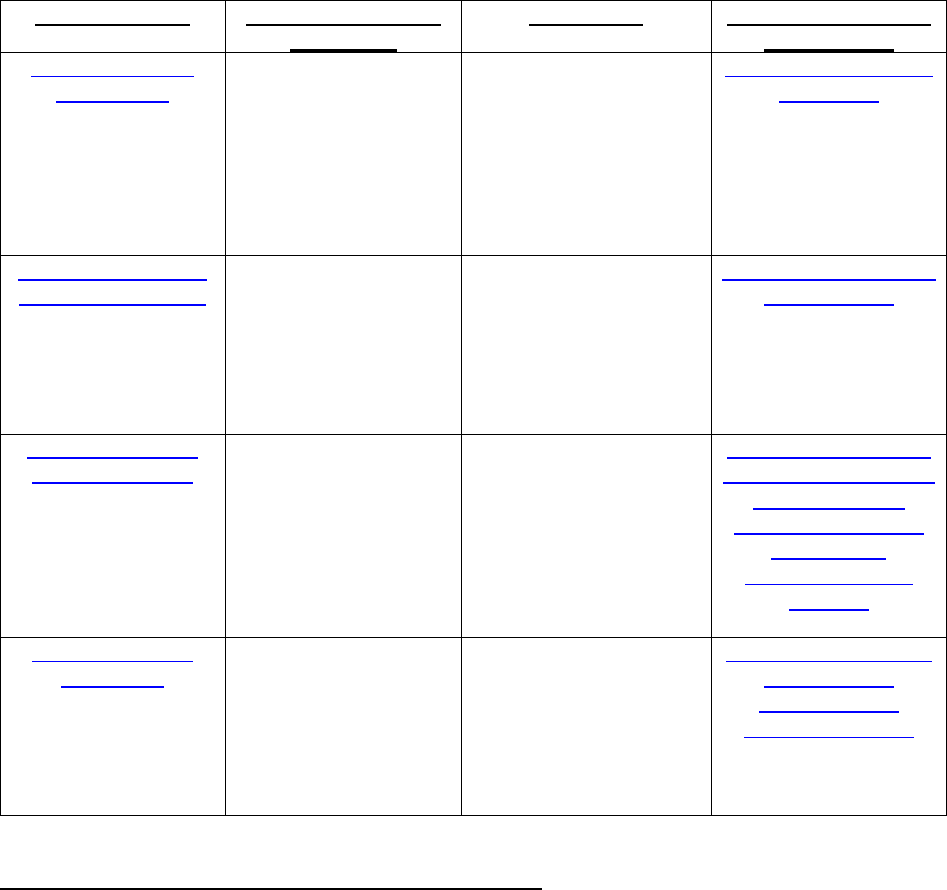
HEALTH PLAN
FIDE SNP NAME &
CONTACT
COUNTIES
ONLINE PROVIDER
DIRECTORY
Amerigroup New
Jersey, Inc.
Amerivantage Dual
Coordination (HMO
SNP)
1-800-374-3631
(TTY 1-800-855-
2880)
Atlantic, Bergen,
Burlington,
Cumberland, Essex,
Gloucester, Hudson,
Mercer, Middlesex,
Monmouth, Morris,
Ocean, Passaic,
Somerset, Union
http://amerigroup.pris
misp.com/
Horizon Healthcare
of New Jersey, Inc.
Horizon NJ TotalCare
(HMO SNP)
1-800-543-5656
(TTY 711)
Atlantic, Cumberland,
Essex, Gloucester,
Hudson, Hunterdon,
Mercer, Monmouth,
Morris, Passaic,
Salem, Somerset,
Sussex, Union, Warren
http://doctorfinder.hori
zonblue.com/
UnitedHealthcare
Community Plan
UnitedHealthcare
Dual Complete ONE
(HMO SNP)
1-800-514-4911
(TTY 711)
Atlantic, Bergen,
Burlington, Camden,
Essex, Gloucester,
Hudson, Mercer,
Middlesex, Monmouth,
Morris, Ocean,
Passaic, Somerset,
Union
http://www.uhccomm
unityplan.com/nj/medi
care/2017/dual-
complete-hmo-snp-
one/lookup-
tools.html#find-a-
provider
WellCare Health
Plans, Inc.
WellCare Liberty
(HMO SNP)
1-877-706-9509
(TTY 1-877-247-
6272)
Bergen, Essex,
Hudson, Middlesex,
Morris, Passaic,
Somerset, Union
https://www.wellcare.
com/en/New-
Jersey/Find-a-
Provider#/Search
Aetna does not offer a FIDE SNP option at this time.
What should I do in an emergency, or if I have an urgent need for hospital services, medical
supplies or equipment?
Last update: 2/10/2017
A: For emergency care needs, please call 911 or go to the nearest emergency room. If you are
switching to a FIDE SNP and you have an urgent or ongoing need for hospital services, medical
supplies, or equipment, be sure to contact the SNP in advance to make them aware of your needs. All
of your hospital services, medical supplies and equipment will soon be provided by your new plan, but
during your transition the FIDE SNP plan will reach out to your old health plan to help transfer care
records, prior authorizations, and prescriptions to ensure continuity of care.
Am I going to be able to keep my current durable medical equipment (DME), e.g., hospital bed,
wheelchair, etc.?
A: If you are currently using DME: Ask your current DME provider if they participate with the FIDE
SNP. If they do, you can continue to use your current DME, and no change will be needed. If they
don’t (and you still plan to enroll), the FIDE SNP can assist you in finding a participating provider. You
will be able to keep your current DME while you are making the transition into the FIDE SNP.
If I enroll in a FIDE SNP, how quickly can I talk to the new care manager?
A: The fastest way to contact a care manager for the first time is to contact the plan’s customer service
line and request care management. Also, please participate in the plan’s health risk assessment. It is a
short questionnaire that helps the plan determine the level of care management that is right for you.
Your care manager is assigned by the plan upon completion of the health risk assessment. For MLTSS
members, please see the section called MLTSS under FIDE SNP.
How do I get a prescription filled or pharmacy services in my new FIDE SNP?
A: Your new FIDE SNP will help you transfer all your pharmacy information, including authorizations so
you can continue to obtain your needed prescriptions. Your FIDE SNP will assist you with prescriptions
and pharmacy services.
MLTSS under FIDE SNP
In 2016, New Jersey began offering all managed long-term services and supports through the FIDE
SNP. MLTSS services for eligible individuals are coordinated with Medicare and Medicaid services by a
single care manager.
All FIDE SNP plans offer the full scope of Managed Long Term Service and Supports (MLTSS)
benefits, including Home and Community Based Services, for members who meet MLTSS clinical
and financial eligibility criteria.
Some frequently asked questions regarding MLTSS under FIDE SNP are addressed below:
Q: How can an existing FIDE SNP member gain access to MLTSS benefits?
A: A FIDE SNP member has the option to speak with their Primary Care Provider or FIDE SNP
plan Care Manager to initiate the assessment process to determine MLTSS eligibility. A
member can also call their plan’s customer service number to request assessment (please see
the chart on page 3 for contact information).
Q: How can an existing MLTSS member (who is not currently a FIDE SNP member) join a FIDE
SNP plan?
A: Any interested MLTSS member should contact the FIDE SNP plan directly. (Keep in mind that
FIDE SNP plan availability varies by county and not every NJ FamilyCare Plan offers a FIDE
SNP.) MLTSS members may keep their MLTSS care manager if they enroll in their current
plan’s FIDE SNP option.

Last update: 2/10/2017
FIDE SNP Enrollment and Disenrollment
FIDE SNP Enrollment Tips
• You can select a new Medicare FIDE SNP plan by calling 1-800 MEDICARE (1-800-633-4227,
TTY#: 1-877-486-2048), 24 hours a day, 7 days a week. At www.Medicare.gov
, you will find a
Medicare Plan Finder that will let you know which FIDE SNP plans are available in your county.
• For more personalized assistance, you can contact your local State Health Insurance Assistance
Program (SHIP) office at 1-800-792-8820. They will help you select a new plan. You will then have
to contact your new plan or call 1-800 MEDICARE (1-800-633-4227, TTY#: 1-877-486-2048)
available 24 hours a day, 7 days a week, to enroll in the new plan.
• NJ FamilyCare members enrolled in Medicaid under the Medicaid Expansion rules under the
Affordable Care Act (for adults with income between 100% and 148% of FPL, PSC 762) are not
eligible to enroll in the FIDE SNP when they become eligible for Medicare. Once a Medicaid
Expansion member qualifies for Medicare, he or she will be notified by the State that their NJ
FamilyCare coverage will end. They should contact their local county Board of Social Services (also
known as County Welfare Agencies) for more information on qualifying for traditional Medicaid
through the Aged, Blind and Disabled Program. Please follow the link to see a list of county
agencies: http://www.nj.gov/humanservices/dfd/programs/njsnap/cwa/
. These members should also
contact SHIP (1-800-792-8820) for more information on programs to assist with payment of
Medicare premiums and Extra Help for Part D Medicare Prescription Drug costs.
What happens if, after becoming a member of a FIDE SNP, I want to disenroll?
• You can choose original Medicare (fee for service). You can call Medicare at 1-800 MEDICARE
(1-800-633-4227, TTY#: 1-877-486-2048) available 24 hours a day, 7 days a week, and ask to be
enrolled in Original Medicare and a Medicare Part D prescription drug plan. If you take no further
action, you will automatically be enrolled into the NJ FamilyCare plan associated with your FIDE
SNP MCO. If you wish to select a different NJ FamilyCare plan, you can call NJ FamilyCare
(Medicaid) at 1-800-701-0710 (TTY#: 1-800-701-0720).
• You can also choose to enroll in a Medicare Advantage Prescription Drug Plan. For this option you
should call 1-800 MEDICARE (1-800-633-4227, TTY#: 1-877-486-2048). However, please be
advised that there are costs associated with other (non-SNP) Medicare Advantage plans that
do not exist with FIDE SNP plans. If you take no further action, you will automatically be enrolled
into the NJ FamilyCare plan associated with your FIDE SNP MCO. If you wish to select a different
NJ FamilyCare plan, you can call NJ FamilyCare (Medicaid) at 1-800-701-0710 (TTY#: 1-800-701-
0720).
• You can disenroll from your current FIDE SNP and enroll in a new FIDE SNP simply by requesting
enrollment in a new FIDE SNP. You will automatically have all Medicare, Medicaid, and Prescription
Drug services switched to your new FIDE SNP on the first of the month after you ask to change
plans. You can do this by contacting Medicare (1-800-633-4227, TTY#: 1-877-486-2048), 24 hours
a day, 7 days a week), going online to Medicare.gov’s planfinder by using this link:
Enrollment in a FIDE SNP is completely voluntary. No one is required to enroll. If
your health plan says you must enroll in the FIDE SNP, please contact the State
Medicaid Hotline to report it: 1-800-356-1561.

Last update: 2/10/2017
https://www.medicare.gov/sign-up-change-plans/index.html
, or by contacting one of the plans on
page 3 directly.
• If you are planning to disenroll from FIDE SNP and enroll in PACE (Programs of All-Inclusive Care
for the Elderly) it is strongly recommended that you follow the process described below:
o You should first determine if PACE is available in your community. PACE coverage areas are
designated by zip codes. The page at the following link includes a list of PACE coverage areas
by zip code: http://www.state.nj.us/humanservices/doas/services/pace/
o You should then contact the PACE site for your coverage area to determine if you are eligible
and arrange for enrollment. The page at the link above also includes contact information for
each PACE site.
o Because you cannot be enrolled in FIDE SNP and PACE at the same time, you should then
contact Medicare at 1-800 MEDICARE (1-800-633-4227, TTY#: 1-877-486-2048) or
Medicare.gov to disenroll from FIDE SNP. You must be sure that your disenrollment from FIDE
SNP takes effect the day before your enrollment in PACE takes effect (for example: for a PACE
enrollment starting February 1
st
, FIDE SNP disenrollment should be effective January 31
st
). You
should ask both your Care Manager and the PACE provider to assist you in coordinating this
process.
What happens if I just call NJ FamilyCare (to disenroll from FIDE SNP)?
• You would not be able to make any actual changes through this method, and would eventually be
directed to contact either Medicare or your current FIDE SNP Plan to disenroll. Only Medicare or
your FIDE SNP Plan can initiate a disenrollment.
State Health Insurance Assistance Program (SHIP)
State Health Insurance Assistance Program (SHIP) provides free, unbiased help in selecting Medicare
health and drug plans. If you need assistance with your decision to enroll in a DSNP verses Original
Medicare or other Medicare health and drug plans options, call the state SHIP hotline to be referred to a
local counselor. The SHIP hotline number is 1-800-792-8820.
