
Colby College Colby College
Digital Commons @ Colby Digital Commons @ Colby
Honors Theses Student Research
2022
The New Mainers: An Exploratory Analysis of Healthcare The New Mainers: An Exploratory Analysis of Healthcare
Experiences in the Somali Bantu Community Experiences in the Somali Bantu Community
Jordan R. McClintock
Colby College
Follow this and additional works at: https://digitalcommons.colby.edu/honorstheses
Part of the Public Health Commons
Colby College theses are protected by copyright. They may be viewed or downloaded from this
site for the purposes of research and scholarship. Reproduction or distribution for commercial
purposes is prohibited without written permission of the author.
Recommended Citation Recommended Citation
McClintock, Jordan R., "The New Mainers: An Exploratory Analysis of Healthcare Experiences in
the Somali Bantu Community" (2022).
Honors Theses.
Paper 1384.
https://digitalcommons.colby.edu/honorstheses/1384
This Honors Thesis (Open Access) is brought to you for free and open access by the Student Research at Digital
Commons @ Colby. It has been accepted for inclusion in Honors Theses by an authorized administrator of Digital
Commons @ Colby.

The New Mainers: An Exploratory Analysis of Healthcare Experiences in the
Somali Bantu Community
An Honors Thesis
Presented to
The Faculty of the Department of Science, Technology, and Society
Colby College
In partial fulfillment of the requirements for the
Degree of Bachelor of Arts
By
Jordan Rhyse McClintock
Waterville, Maine
May 13, 2022
1

Signature Page
Examined and Approved on
By
Advisor
Department Chair
Reader
2

Abstract
Healthcare inequities within the United States’ Western model of medicine have
existed for hundreds of years. The purpose of this year-long project was to analyze the
existing qualitative and quantitative studies of healthcare barriers for the Southern Maine
Somali Bantu population, as well as compiling narrative pieces from Maine
non-governmental organizations that provide community resources. In doing so, the idea of
healthcare access and literacy was analyzed through means of understanding systemic
barriers. Overall, the findings of this exploratory project point to a lack of cultural humility
within medicine, the importance of recognizing intersectional identities in quality of
healthcare, and the usage of healthcare literacy as a means for the healthcare system to
exclude the Somali Bantu community from receiving equitable care.
3

Acknowledgements
I would like to thank Dr. Ashton Wesner for her continued guidance and support
throughout the academic year. Without her, I would never have been able to reach deep
within myself and create a project that encapsulates my history and the amazing healthcare
advocacy work being done for marginalized communities. Another thank you to Professor
Aaron Hanlon for providing academic support as my STS departmental advisor; he and
Professor Wesner definitely believed in me more than I did in myself. A further thank you to
Professor Nadia El-Shaarawi for being my outside reader and being one of the first to
introduce me to the New Mainers generation, as well as their experience with access to
healthcare. To my wonderful STS seniors, thank you for the valuable feedback and the
motivation during class periods. I would also like to give a huge thanks to Mohammed
Hassan from the Main Immigration Access Network (MAIN) and Muhidin Libah of the
Somali Bantu Community Association for their invaluable anecdotes about empowerment
and advocacy within the Somali Bantu healthcare experience. Lastly, I would like to thank
my mother Jenssie Flores-McClintock for not only inspiring my thesis but inspiring me to
continue advocating for healthcare rights in marginalized communities. Her incredible and
moving story as a displaced child arriving in the United States without healthcare advocates
is a testament that change must happen.
4

Table of Contents
Table of Contents 5
Introduction 6
Literature Review 9
Methods 14
Anecdotes 28
A Field Analysis of Maine Access Immigration Network 31
A Field Analysis of the Somali Bantu Community Association 39
Conclusion 42
Bibliography 44
Appendix A: Outreach Materials 51
Appendix B: Somali Healthcare Infographics 54
5

Introduction
A History of Somalis in Maine
Violence, prejudice, and injustice. All are rooted into the history of the Somali
Bantu people and the stigma surrounding their forced enslavement. In the late 20th
century, a civil war broke out in Somalia and the Bantu group was immediately targeted.
For historical context, the Bantus are a minority group in Somalia that have been
discriminated against for being culturally, ethnically, and socially different from the
majority Somali group. As early as the 16th century, ancestors of the modern-day Bantu
groups were forcibly brought from Zanzibar as enslaved laborers on plantations. The
effects of colonization were apparent in the treatment of the Bantus in the years to come.
Italy, which gained control of Somalia in the late 19th century, had made the state a part
of the protectorate Italian Somaliland and allowed for the continued enslavement of
Bantus in agricultural labor.
Due to the years of stigma surrounding the Bantus, the Italians also treated Bantu
as inferior to the ethnic Somalis. Feelings of negative sentiment and animosity had
perpetrated violence for centuries and it came to a sudden head in the late 20th century. In
the aftermath of the Cold War, Somalia’s dictator-president Siad Barre had nationalized
land, which disenfranchised Bantu farming communities across Somalia. His plans to
invest in different areas across Somalia through educational, infrastructural, and
healthcare reforms tactically excluded Bantu-centered areas. Barre’s reign in Somalia was
6

marked by turmoil and his relationship with the United States directly affected the
country’s stability. The United States had provided military and economic support to
Somalia due to its strategic position in terms of its location between the Persian Gulf and
the Indian Ocean (SBCA). After the fall of the Berlin Wall, the United States severed all
support to Somalia and Barre was forced to abdicate power to anti-government coalitions
and fled to Kenya. The Bantus, under Barre, had faced prejudice in all forms but his
military support had somewhat quelled extremists who sought to target them. With his
government left in shambles, the Bantus were the first to be targeted. The Somali Civil
War yielded heinous war crimes that, to this day, have not been given proper attention
within the international justice system. At the time, it was identified as, “The worst
humanitarian disaster in the world today” by the former director of the U.S. Office of
Foreign Disaster Assistance Andrew Natsios. Bantu families were forcefully evicted from
their land and subjected to cruel and violent torment. Between anti-government militia
movements and famine, the Bantus were forced from their homes and displaced both
physically and mentally. Many of them fled across domestic borders towards Kenya.
Even more fled the African continent and found temporary placement in other countries.
Families looked towards the United States and, after months of research, ultimately chose
Maine (MAIN).
The United States’ most northern state was an ideal relocation because of low
crime rate, affordable housing rates, and structured education. Here, the Somali Bantu
community could start fresh after being faced with violent backlash in their home
country. When they traveled 7,237 miles away to the greater Lewiston area, what they
7

found was a little more than they bargained for (Iftin 2015). They arrived in the New
England metropolitan area and were immediately met with obstacle after obstacle as they
tried to settle within the new healthcare system. Families, young adults, and elderly all
struggled to find and access safety nets of hospitals, clinics, and other providers. The
question that came about was: How could the United States accept a community of
people that they could not- and would not- provide equitable access to healthcare for?
Structurally, United States healthcare is built upon a bureaucratic system of an established
hierarchy that prioritizes market-based regulations and lacks the ability to provide
universal quality care for even its citizens.
In terms of the Somali Bantu community of Maine, the important questions
regarding healthcare access and literacy can become convoluted in regional policies and
dominant hegemonic narratives. In approaching their healthcare experiences, there can be
a few derived hypotheses.
Firstly, Somali Bantu healthcare literacy and access is affected by the systemic
prejudice present in the domestic healthcare system. This looks like a few different
things; there is the way providers are trained in medical school in terms of excluding
intersectional education and considering the differences between patients. There is also
the idea of community healthcare workers not being available in quantities to meet the
needs of the Somali Bantu community.
The second piece surrounding the focus of the thesis is healthcare literacy being
used as an “othering” technique by the system, which produces the highlighted barriers of
this paper. Essentially, health literacy is the ability of an individual to understand and
8

navigate their health options and navigate. In terms of the Somali Bantu community, it is
used as a way to alienate them further from general healthcare access. Rather than
reconcile with the reality that literacy coincides with transparency and access from the
providing government, it is used as a way to blame and reinforce the existing barriers. In
terms of the Science, Technology, and Society role on how to address this plight and its
role within a medical setting, there is the societal aspect of ingrained medical racism that
affects access and health literacy. On a larger scale, the technology piece of how language
translation and other intersectional health techniques could be utilized to create a more
equitable healthcare system. Piecing together the different aspects that surround the
Somali Bantu community’s healthcare experience, this thesis is a contextual analysis of
the healthcare experience and how the industry disadvantages The New Mainers.
Literature Review
Identifying and Categorizing General Barriers
Concerning the framework of my project, some of the cornerstones include
Central Maine publications. The Bowdoin-based CORE piece overviews some of the
most important aspects of my research, including the facets that exclude the Somali
Bantu community from healthcare options on both a regional Maine and national level. It
9

is the framework of my own research in terms of what questions I asked. It offers
valuable stakes in the argument because it provides contacts I utilized within my field
research. In addition to providing insight on the Maine-based healthcare system’s
relationship with the Somali Bantu community, it analyzes the substandard provider
training available. This is where Warwick Anderson’s piece on “Teaching Race in
Medical School” comes into play as an important STS perspective in the difference
between race and ethnicity in medicine. The fine line is seldom understood by providers
and can serve as an additional barrier to marginalized patients. This aspect in my
literature review can be tied nicely together with the work of Hayley Fitzgerald, who
discusses the six main stressors on Maine-based Somali Bantus; “economic stressors,
discrimination, difficulties with acculturation due to language differences, parenting
differences, and pressure to find employment.” Together, these pieces bring together a
resulting analysis that coupled with my own research.
Healthcare Narratives
The backbone of my research centers around narratives from Somali residents
themselves about what they have experienced. Northeastern University- based Ashley
Houston conducted a study on young Somali adults trying to make their way through a
broken system that gives tremendous insight on how there are inequities that contribute to
the societal hierarchy. Houston’s piece shows that there is inequity for those of median
age. Additionally, this section of my research is where autobiographies play a very
10

important role in shaping these types of experience. They also helped supplement
arguments posed by publications that focused on Somali Bantu mothers, who had
valuable commentary on provider’s verbal etiquette. Abdi Nor Iftin’s acclaimed
autobiography details a young man’s journey to Yarmouth, Maine amidst the turmoil of
his home country and new country. His struggles within the system give narrative
perspective on what the studies show through logistics. After interviewing the
agricultural organization the Somali Bantu Community Association, Iftin’s unfamiliarity
with the United States’ frigidity towards identity becomes clear with the system’s
inability to shift towards more open conversations about healthcare access and literacy.
Cultural Humility: A Lack of Compromise in the Western Medical Model
The word cultural humility was not officially recognized until the late 1990s. As
the Boston Medical Center explains in their Policy and Industry piece, cultural humility
“involves understanding the complexity of identities - that even in sameness there is
difference- and that a clinician will never be fully competent about the evolving and
dynamic nature of a patient's experiences”. In approaching medicine with this mindset,
ideally, there will be a reduced amount of bias within practicing medicine because of the
physician’s awareness of their own implicit prejudices. While not a perfect solution to the
large abyss that is health inequity, it does allow for physicians to somewhat embrace both
11

sides of the provider-patient interaction through an understanding of identities. In terms
of the patient, it recognizes what the patient needs as opposed to the mentality that
provider training is flawless.
A valuable piece that offers up an interdisciplinary approach in recognizing what
is important to the patient in healthcare is “Caring for Somali women: implications for
clinician-patient communication” by Jennifer Caroll and a Rochester-based team that
interviewed 34 Somali women in Rochester, New York. This study focuses on the
alternatives for the existing Western medical model that excludes BIPOC individuals-
including women- that may offer potential solutions to the obstacles faced. Increased
patient-provider interaction, which included language interpretation and health literacy
within the clinical setting were found to be successful cornerstones. It couples well with
Susan Bell’s piece on how language interpretation in clinical settings was very effective
in fusing together provider-patient relationships within Somali Bantu communities. This
type of tool is very important in healthcare because being able to understand the patient
in every sense of the word can allow for a more efficient procedure. An interesting part of
the alternative side of medicine comes through the integration of more healthcare workers
within the Somali Bantu community that are designated as community health workers
(Cowenhoven 2017). With this, it is important to understand what a community
healthcare worker is. A large umbrella term, community health workers wear a few
different hats. They are often synonymous with outreach workers, family advocates,
health educators, medical liaisons- among other titles. Essentially, their job is to connect
marginalized communities with health organizations and clinics. They may provide
12

translation or interpretation services and are a pipeline to different health. What this
recommendation brings is a fascinating perspective where perhaps MD and DO
practitioners should not be at the forefront of health. It should in fact be workers who are
trained in specific Somali Bantu healthcare.
From a historical point of view, the Black Panther Party’s creation of the Peoples’
Free Medical Clinics was something that resonated with some of the opinion pieces
within my research. In a sense, the people run the medical system and do it in spite of the
existing hegemonic system. While the situation between The Black Panther Party and the
Somali Bantu community differ in historical context, they have the same issues present.
That being there was a lack of support and specialized care from the government for
Black bodies, which meant there were people needing to take community healing support
into their own hands. As of right now, there is no universal model of medicine that is
conducive to all different races and ethnicities. Particularly in the United States, the
medical industry thrives on making sure all practices and training are completely
uniform. With uniformness comes a lack of recognizing identity.
Fatuma Hussein of the Immigrant Resource Center of Maine and the United
Somali Women of Maine stated it perfectly when she discussed the idea of community
and ancestral healing finding a balance with Western healthcare in her keynote lecture at
the University of New England. The way Fatuma looks at it, when a child is fussing or
does not feel well- parents may read the Quran to them as a way to facilitate the
community’s spiritual healing. In the Western version of healthcare, culture is not
embraced as a factor into how healthcare or wellness is perceived. Spirituality and
13

community healing is not embraced within medicine, which is not only challenging for
different marginalized communities to understand but, it also perpetuates the idea that
there is only one right way to practice medicine and understanding your patient is not at
all something to consider nor think about.
Methods
A General Overview of Literature Analysis
Analyzing existing studies that encapsulate healthcare inequities through
quantitative and qualitative data, I also consulted Maine non-for-profits, governmental
organizations, and representatives from the Somali Bantu community. Combining both
into a capstone project that looks at barriers through an STS lens of how advancing
medical practices still exclude marginalized communities through inadequate provider
training. In terms of procedure for my study, I analyzed existing studies that specifically
look at different experiences in the Somali Bantu community. Anecdotal evidence points
to the idea that Somali Bantu community members within the Southern Maine area have
experienced healthcare experiences. From families, young adults, to elderly, it is clear
across the board that there are discrepancies in the quality and security of their
healthcare. Identifying different commonalities across each correspondence and
identifying the most prevalent barriers and how they structure into healthcare
14

experiences. Each representative received a flexible questionnaire with guiding questions
that allowed for a more informal conversation to take place. The latter was centered
around a few central questions that coincide with my research hypotheses: In terms of
identities, do Southern Maine healthcare providers have training that specializes in
cultural humility? Describe the differences in obtaining clinical care within the Somali
Bantu community between someone with documentation and someone without. What
does representation look like in terms of care providers that speak Somali? These
inquiries helped loosely guide their responses for insight into the healthcare experiences
of Somali Bantus as providers and non-for-profits giving aid.
A Global Perspective
2000 was the year of a new millennium. Commerce, technology, and infrastructure
was advancing at a rapid rate. Consequently, it was also the turning point in the Somali
Civil War, which had begun in 1991. As previously discussed, the overthrow of the
government resulted in tens of thousands displaced Bantus from their land by militia
forces. The resettlement of Somali Bantus in the United States was a whirlwind of
activity, as about 1,000 of them set their sights on Southern Maine (Huisman 2011). Upon
their arrival, a term that was used to describe the growing Somali Bantu population in the
small cities stretching across inland and coastal Southern Maine was “The New
Mainers”. Referencing their recent settlement and new contribution to Maine’s social and
15

cultural profile, it became used to reference the new generation of Maine inhabitants that
would share their experience with the domestic community and attempt to start a new
life.
When fleeing your home country to settle in an unfamiliar one, there is already an
immense amount of pressure. Adding the additional worry of how you will be perceived
in a medical setting is almost unimaginable. Now, in terms of medicine, what are the
inequity factors that drive the resulting biases in medicine?
Nina Sun discusses in her piece, “Human Rights and Digital Health Technologies”
how digital health technologies can contribute to expanding health inequity, widening the
“digital divide” that separates those who can and cannot access such interventions”.
What this entails is that racial biases perpetuate racial grouping and stereotyping that
affects the type of care they can receive. This idea is not a tangible one but, after
conducting my own research, was revealed through correspondence with the
organizations.
Referring to Figure 1, the difference between race-based medicine and
race-conscious medicine can be determined. The type of model that we use in the United
States is centered around race-based medicine. This type of idea referring to race as a
medical technology is something that my colleague Fariel LaMountain explored further
in her thesis. From a STS point of view, the idea of race in medical school is something
that factors heavily into how people are equipped for care. Warwick Anderson’s
“Teaching `Race' at Medical School” is an interesting look into how race and ethnicity
are often two synonmyous terms that are not usually understood. Anderson offers up the
16
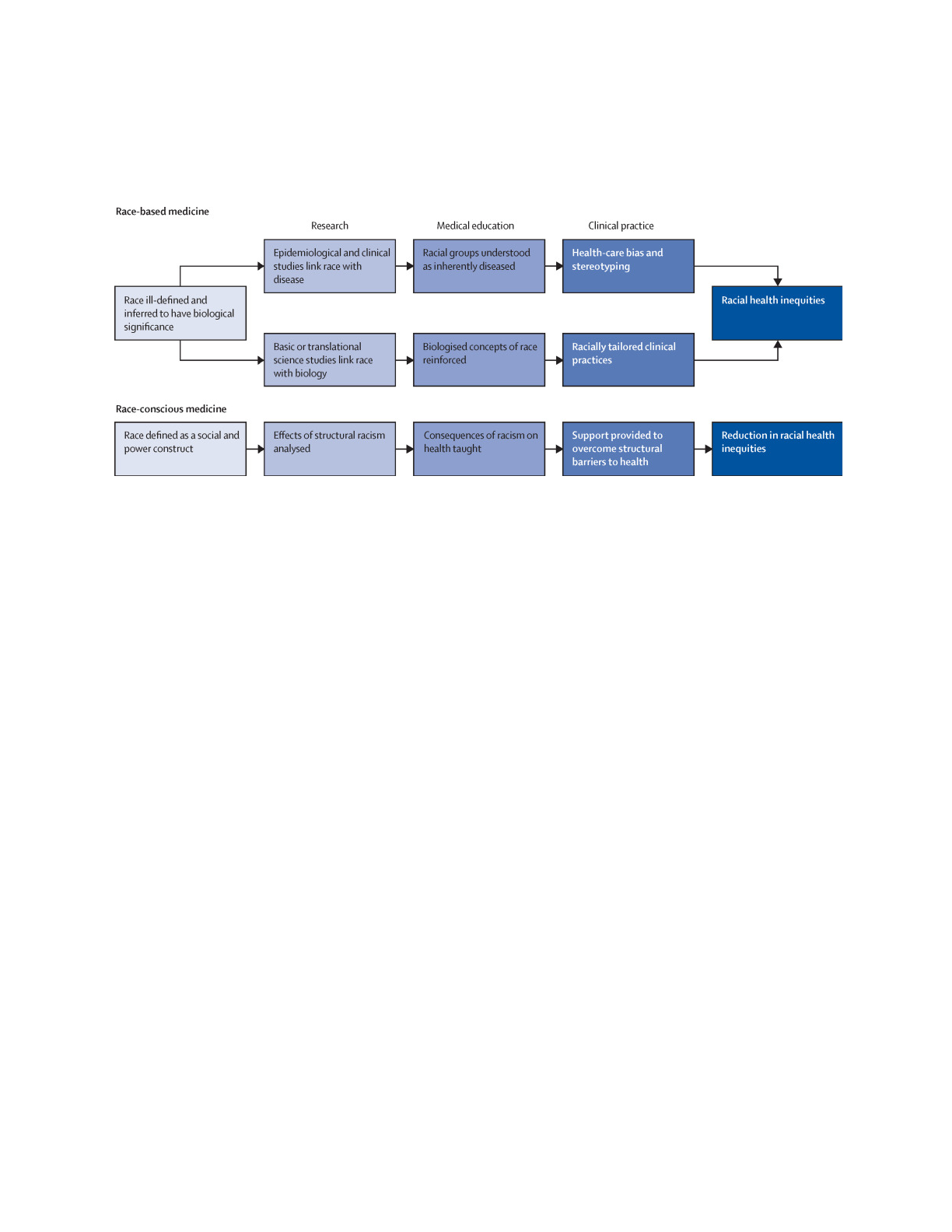
notion where because of this, there is a lack of understanding concerning how people
need to be treated with this type of identity in mind.
Figure 1. A diagram that shows the difference between race-conscious medicine and race-based medicine. The idea
is to have one recognize social constructs and have providers engage in cultural humility with a recognition of
system biases.
Cerdeña JP, Plaisime MV, Tsai J. From race-based to race-conscious medicine: how anti-racist uprisings call us to
act. Lancet. 2020 Oct 10;396(10257):1125-1128. doi: 10.1016/S0140-6736(20)32076-6. PMID: 33038972; PMCID:
PMC7544456.
Thus, the small state of Maine unfortunately experiences this trickle down effect in
healthcare policies because of the societal racism that is deeply ingrained. In terms of
what types of experiences are happening in Southern Maine, there is a very good insight
in what occurs through studies done by Northeastern institutions. Ashley Houston’s
research based from Northeastern overviewed young Somali adults with ages ranging
from late teenage to adult years. Within the healthcare system, they were not afforded
equal opportunity because of socioeconomic boundaries that centered around cost. It was
17

clear that provider training did not contain any kind of cultural humility, or a respect and
understanding of different aspects of a person’s identity.
This study is not the only look into the types of barriers that exist. There are a few
other qualitative and quantitative studies that not only identify barriers but also look into
how there are alternative models for facing these issues. The truth is that the current
model is ineffective because it refuses to help marginalized communities which, in turn,
continues to perpetuate violence against non-white communities. The first thing that is
important to note about the barriers is that they can be summed up into four main
categories.
A large one is the national health care system, which of course offers a strict
criteria that cannot always be met because of documentation status. This is something of
note within the Somali Bantu community because there are different situations for
different individuals. There are three types of classifications that determine health
resources from not only the national level but the Maine level (Agrawal 2016). This
project is a cumulative analysis of the healthcare experiences through access and literacy
of the entire Somali Bantu community however in terms of what is available, it differs
between those who have specific status over others. This is the reality of Western
healthcare so, it is important to acknowledge this aspect in the overall thesis.
Figure 2 is a visual representation of what this difference looks like through a
metaphoric hierarchy. Refugees have access to national healthcare, regional healthcare,
and most public insurances with benefits for employee security. They are given this
refugee status while still outside the United States and sponsored. Asylum seekers are
18

different in that they have been status at the point of entry or after entering their new
country. They are afforded less health care opportunities than refugees in that they are
able to have regional healthcare for minors but not entire families nor are they able to rely
on employee benefits (Xin 2018). The last are undocumented individuals, who have
extremely limited access to federally funed programs.
There is a national crisis in terms of undocumented folx not receiving proper care.
According to the United States Department of Agriculture, “53% of domestic
farmworkers” and laborers are undocumented. Those who utilize the existing medical
system hover between 38% and 53%. What this entails is undocumented folx, including
those in the Somali Bantu community, being afraid or untrusting to utilize resources. This
comes as no surprise, as there is generational distrust within marginalized communities
because of the systemic racism present within our healthcare system.
19
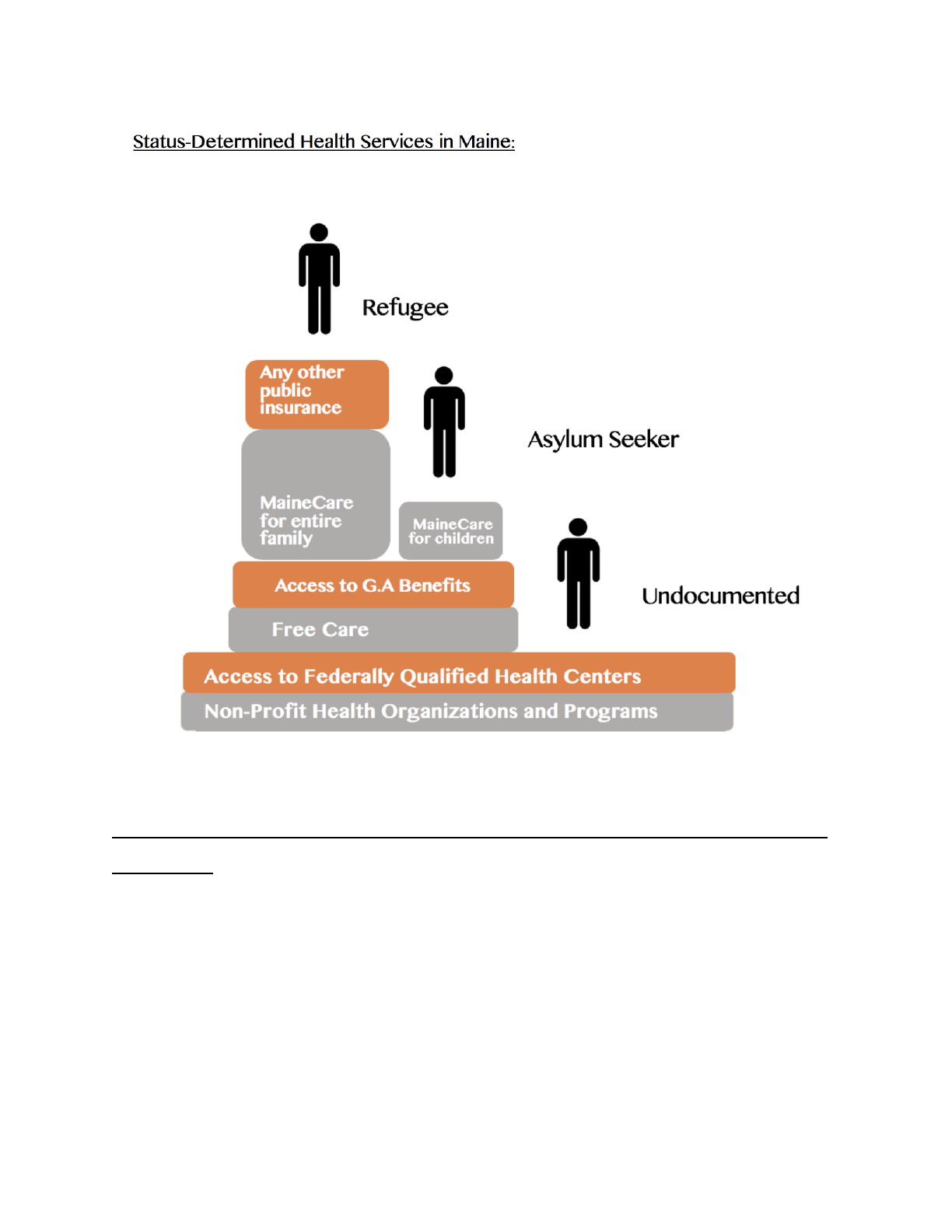
Figure 2. This diagram shows the designations between refugees, asylum seekers, and undocumented folx.
https://community.bowdoin.edu/news/wp-content/uploads/2018/10/Major-Barriers-to-Healthcare-Access-for-New-
Mainers-2-1.pdf
What makes this so complicated is that all three exist within the Somali Bantu
community and all three receive different levels of care. Something that was very evident
within the narratives of both Cynthia Anderson and Catherine Besteman’s novels was that
there are adjustments for not only those displaced but, those who live in communities that
20

gain new neighbors over a period of time. This type of societal reaction is something that
also factors into the psychological factor of receiving healthcare. In short, because there
are sometimes push backs against displaced individuals inhabiting a new place, it can
trickle into the quality of healthcare received. For example, within the initial surface
research conducted, there was not a percentage available of healthcare providers that
could speak Somali and engage with different aspects of their patient’s documentation
status, gender identity, income, health conditions, family accomodations, and other
aspects. Language is extremely important in giving healthcare to marginalized
communities and Bell’s piece ties in how it is so important to directly understand a
patient’s symptoms, which can be hard to do if that is a barrier.
Another layer is gender identity’s representation in the healthcare field. Jennifer’
Caroll’s overview of Somali women and a study about patient communication found that
many of the Somali women preferred having a female identifying provider in the room
during their care. This is something that is often overlooked as a patient necessity but it
factors heavily into the overall quality of care. This was further explored in Hill’s piece
on Somali natal care- specifically how expectant or current mothers have a sense of trust
in their providers when they feel they have a sense of control in their situation. Having a
sense of cultural humility and understanding of intersectionality in the workplace is
something that can be so valuable to caring for another human being.
Additionally, having an element of health literacy between patient and caregiver is
another level of comfort to the parties involved. One study method used is a parameter of
patients’ medical awareness called Patient Activation Measure (PAM). Lower PAM
21

scores from patients reflects a lower health literacy rate. According to a study done, “24%
of Portland respondents had a Level 1 score”. Level 1 is the lowest score and is indicative
of the fact that marginalized Portland communities could greatly benefit from community
health workers (Cowenhoven 2017).
Having this would lower stigma in asking for help, as well as prioritizing mental
health. Displacement effects on mental health are large parts of how people can function
in new environments. The 5 stressors that were deduced from mental health effects within
Somali communities were broken down into: “economic stressors, discrimination,
difficulties with acculturation due to language differences, parenting differences, and
pressure to find employment.” (Fitzgerald 2017). Mental health effects of marginalized
folx is something that factors into why organizations like the Black Panther Party
organized their own medical care. Alondra Nelson’s book gives a look into how social
justice and medicine goes hand in hand through the lens of dismantling systemic racism
within the hospital system. While this was decades ago, it does offer an alternative
method into creating a community healing system. Ultimately, what this project entails is
possibly exploring a model that would be better suited for the Somali community.
“Improving the wellbeing of the world’s migrants requires an intersectional lens that
focuses on the diverse circumstances and locations in which migrants are situated”
(Spitzer 2019). In other words, the only way Somali Bantu healthcare will improve is if
an intersectional approach is made.
22

Field Research: Interacting with Maine Healthcare Advocacy Partners
During the research portion of my thesis, I wanted to integrate my own
commentary into the existing literature about the Somali community. Their healthcare
access is something that has been in conversation for a long time. As a precursor, I want
to stress that I was fortunate enough to be privy to some very important anecdotal
narratives from the non-governmental organizations that represent and support the Somali
Bantu community. However, I am simply an academic that had the opportunity to do so
and in no way represent the healthcare plights of the Somali Bantu community. My
overall goal for this thesis was to have an analytical look at their experiences and
hopefully provide a platform to further amplify their voices. The advocacy done by their
community and affiliated associations for a more inclusive healthcare system is beyond
the work that I could possibly do within a year.
During the planning stages of my thesis research, I took inspiration from a few
different peer-reviewed sources in terms of how they conducted field work to collect
narratives regarding Somali Bantu healthcare in the Maine and Greater New England
area. Close attention was paid to what types of questions or hypotheses were being posed,
what specific focus of healthcare inequity was being studied, and how they analyzed their
findings.
23

When thinking about the methods used within my research, something that
distinguished Matteen Hakim’s piece is its presentation format and the fact that it actually
is a student project for a medical student in their rotation during their final year of study.
Hakim’s focus on the Somali community of Southern Maine- specifically Lewiston- and
the different types of barriers within the community parallels my own thesis topic. The
presentation is broken into what problems appear to be, the pecuniary implications of
public health, anonymous community perspectives, the methodology (incorporating
Somali voices into the healthcare narrative), the results (or perspectives given) from
interviews, limitations, and recommendations for future research. This piece was a really
important stake in the methodology because it does have similarities to the way I am
approaching analysis for healthcare barriers. Additionally, it mirrors the interview style of
community outreach that I hope to accomplish in my ethnographic approach to interviews
in the field. One of the main aspects of the piece that I also found to be similar to mine
was the types of people being interviewed and the approach to advocating for community
healthcare workers.The future research area of the presentation was also interesting
because I feel that expanding on the point of increased language accessibility is
something that my project looks at in my written analysis of different barriers. Hakim’s
final product is something that offers great insight on the healthcare provider side of
Somali healthcare literacy and accessibility.
24

As a methodology, it matches up with my vision and also offers up important
potential points about connecting community advocates with healthcare support
organizations for my own research. The second piece that supplements Hakim’s piece and
offers up an interesting perspective for student researchers within the Lewiston area is
authored by three graduates, who had a similar methodology to both me and Hakim in
terms of conducting field research. The one thing that makes it different is its focus on the
transportation access issues of the Somali community, which is something that I had
explored at all within my research. It is something that I feel needs to be explored within
my paper. There are points brought up about not simply just logistic access but, there is
the notion of biases within those who are supposed to provide transportation. There is
also the idea of barriers not being fully understood by domestic-based organizations,
which may not know how to collaborate with community advocates (Caldwell 5).
My thesis is simply a hybrid ethnographic-analytical look at the work they do in
conjunction with the peer-reviewed sources that provide quantitative data. The two main
organizations I had the privilege of interacting with were the Maine Access Immigration
Network (MAIN) and the Somali Bantu Community Association (SBCA). My key
contacts for each were Mohammed Hassan and Muhidin Libah, respectively. Hassan is a
community health worker originally from Somalia and later moved to Syria where he
worked with Somali refugee families. Conversational in over four languages, Hassan has
practiced medicine in Somalia, Saudi Arabia, and partnered with the United Nations High
Commissioner for Refugees in Damascus, Syria. He joined the Portland-based MAIN
specifically to provide care for those that are disadvantaged by the public system because
25

he has a huge commitment to ensuring equal access for all those who do not know how to
advocate for themselves or their families.
Muhidin Libah is the executive director of the Somali Bantu Community
Association in Lewiston. He arrived in Southern Maine around 2001 and grew up in a
Kenyan refugee camp following the Somali military conflict. He attended the University
of Southern Maine and founded several non-for-profits in addition to the SBCA. His
mission upon arriving in Maine was to empower Somalis through land cultivation and a
sense of community. Agricultural wellness is a pinnacle in Somali Bantu culture and
something that was difficult upon arriving in the United States was for the community to
preserve their culture. Referencing back to Fatuma Hussein’s lecture about Western
medicine, there is a separation between patient and provider in the clinical setting that
goes far beyond just medical expertise. When a patient arrives into a space where the
provider giving them catre does not look like them, there is a high chance of implicit bias
concerning that individual’s identity and the care they can receive.
Technical Procedure
To better understand the role of the non-governmental organizations that represent
healthcare advocacy for the Somali community, my original plan was to hold interviews
with organization representatives using either the phone or a virtual software. Before the
interviews, there would be a consent form sent, which is included in this methods section.
During the actual interview, there would be guiding questions that would steer the
26

conversation but give the interviewee full autonomy and treat the prompts as a starting
off point. The questions were structured around understanding exactly what the
organizations do, the role the organization has in the healthcare conversation, the effects
on the Somali Bantu community of the medical training for providers in Maine, and the
overall experience of the Somali community in the United States’ medical system. The
idea behind this type of field research was to combine these collected narratives with the
literature analysis to better prove or disprove some of my hypotheses.
In terms of limitations, there were some challenges that did influence the way I
conducted my research. Due to COVID-19 complications and important work occurring
on a day-to-day basis for the organizations, my interactions were limited to email
correspondence. Essentially, all materials were sent over email and the questions turned
into shorter essay prompts for the representatives to answer. In an ideal world, interviews
would be conducted face-to-face, however, because of health concerns due to the
pandemic, safety had to be prioritized.
Following the correspondence, I was able to compile key points from both
Muhidin Libah and Mohammed Hassan that were incredibly beneficial to my own field
analysis. The following anecdotes from both are direct quotes in response to the
open-ended questions sent to them over email. Incredibly thorough, the answers reflect
my initial hypotheses very strongly in terms of systemic barriers factoring into the quality
of care due to existing prejudice. They also touch upon how healthcare access and
literacy is directly linked to the ease of navigating a system that does not take
intersectionality into account. An interesting aspect of both these organizations is that
27

while their missions are directly linked to forms of healthcare advocacy- whether it be
more resources to clinical care or agricultural health and wellness- they are both
incredibly different. However, their responses to the prompts yield similar themes of
access inequity and the difficulty the Somali community has in terms of a lack of cultural
humility within Western health. This was incredibly fascinating because the organizations
have different missions but nearly the same fundamental values of connecting and
empowering the Somali Bantu community. It is clear within the anecdotes provided to me
from both Hassan and Libah that the healthcare experiences of the Somali Bantu
community and the organizational approach to them operate in a variety of different
ways. For example, the SBCA’s health and wellness commitment through agricultural
empowerment was a wellness initiative that I had never been exposed to. However, after
learning more about the Somali Bantu identity and what the organization does, the
importance of health and wellness through the growing, harvesting, and celebration of
food should absolutely be recognized as a form of healthcare.
Anecdotes
Maine Access Immigration Network (Mohammed Hassan)
Explain a little about what your organization does to support the Somali
Community?
28

“We are a non-profit ethnic based community organization that helps immigrants
who speak different languages including the Somali speaking community in Maine by
providing health literacy educational meetings to communities in partnership with major
healthcare providers, helping newly arriving immigrants access to social services such
healthcare, food, housing and other needs by connecting them to providers in Maine. We
also advocate when needed to certain vulnerable individuals. We partner with providers
to help them perform research projects for the communities we serve”.
What is the experience of a newly-arrived family or individual in terms of obtaining
physicals/general health check-ups?
“Newly arrived Somalis come to the US with different immigration categories
such Refugees, Family Reunion and rarely as Asylum seekers (undocumented) . Free
health care coverage depends which category of immigration they arrive here, those who
enter as refugees can get Medicaid health insurance which covers all health and other
social services at least for the first few months until they earn income while asylum
seekers are not eligible free healthcare coverage except children and pregnant women,
same are also those who enter with family reunion visa”.
How have the communities of Southern Maine transitioned after the arrival of the
Somali community?
29

“Somali communities in Maine experience hardships due to all barriers such as
language, culture, and the weather but they transition from being an immigrant to
becoming hard working individuals with citizenship while their children enroll in higher
education and integrate with the mainstream population and we help them navigate the
complicated American health care system”.
What does representation look like in terms of care providers that speak Somali?
“Healthcare providers are mainly white and do not speak Somali language but,
providers use interpreters although lately MaineHealth is trying to diversify their
residency programs with few Somali providers who speak Somali Language”.
Describe the differences in obtaining clinical care within the Somali community
between someone with documentation and someone without.
“As mentioned above those who legally arrive are eligible to certain level of
service depending income and other factors while undocumented Somalis are not eligible
for state or federal healthcare coverage except emergency medical care that may be billed
to them”.
30

Somali Bantu Community Association (Muhidin Libah)
“Somali Bantus are people who come from rural areas where there were no
hospitals, running water [nor] medical services. When the people came to the USA they
were overwhelmed with many different Western diagnoses and treatments, which were
foreign to our community. The medical reconciliation's mission is to make sure our
people get clear information about the new medical systems.
Somali Bantus were farmers in Africa, they used to live on the banks of the rivers
captivating the land and fishing, hunting, and gathering, farming comes with traditional
healing and treating diseases, farming was not only producing food, but it was also a way
of life. Everything was around farming”.
A Field Analysis of the Maine Access Immigration Network (MAIN)
The mission of MAIN is to “[address] refugee/asylee health literacy, health care
enrollment, and coordination of health care services”. They are funded by the Office of
Refugee Resettlement Ethnic Community Self Help Grant, the Maine Health Access
Foundation and the Maine Community Foundation. Partners they have around Maine are
Greater Portland Refugee and Immigrant Health Collaborative, University of New
England CHANNELS Project, Care Partners, MaineHealth, and Mercy Hospital.
Renowned for its commitment to providing a bridge between marginalized communities
31

that are newly settled in Maine and health resources and practices around the state, its
staff are passionate about making access more available. Their executive staff were all
new to Maine and its health systems so, they have a deeper empathic understanding of the
Somali Bantu community’s struggles. Their organization was one that immediately struck
me as an important outlet to consult because of the staff’s personal connection to
healthcare access, the vast resources they provide, and their plethora of community
healthcare workers available.
Mohammed Hassan is one of these community healthcare workers and he was able
to provide me with more context about MAIN and the different experiences that occur in
the healthcare system. One thing that MAIN does to address the issue of literacy and
access is providing educational meetings for those that need assistance navigating the
healthcare system. As Hassan articulated, when new arrivals enter the state of Maine,
they immediately become a number. Everything depends on status and even those who
enter Maine with some type of citizenship do not always qualify for benefits. Something
that was quite shocking that Hassan revealed was the fact that emergency services are
often the only qualified medical care for the Somali community and yet they are often
billed for it. This goes hand in hand with the idea of rooted systemic prejudice affecting
the care they can receive. Even though there are those in the Somali Bantu community
that technically qualify for Medicaid and regional healthcare, these benefits are short
term and financially unreasonable.
32

Even more limiting are the opportunities for undocumented members of the
greater Somali community. Referencing back to Darlene Ineza’s study, a direct quote
from a Maine-based physician is that “Undocumented don’t have a voice at all. In my
experience, I have never seen any undocumented patients” (18). This is echoed within
Hassan’s conversation with me; in my field research I was unable to obtain many
resources directly available to not only the undocumented members of the Somali Bantu
community but, all of Maine’s minority communities. No doubt this is a structural issue
overall in the United States, however, it seems so much more apparent in Maine because
of the state’s lower population density. The reality of the benefits available federally for
newer arrivals is that there are far and few between. Hassan’s experience is primarily
centered around connecting health services with Somali Bantu community members who
seek out guidance. Something that Hassan also does is being responsible for combing
through Maine healthcare legislation in order to better understand how best to help the
Somali Bantu community members based on their situation. This, I argue, is just another
reason why community healthcare workers are so important to marginalized
communities.
As explained in Warwick Anderson’s medical education training piece, there is so
much risk for biases when providers are simply given the general medical training that
operates on nearly a purely academic-level. There is no incorporation of socioeconomic
identity when treating patients, which is why initiatives such as the Black Panther Party’s
community clinics arose. There is so much room for error in treating patients that do not
33

have the same identity as their provider. In terms of my first hypothesis about prejudicial
influence on healthcare access and literacy, this was a watershed moment that occurred
during my research. It made me realize how far the roots of racism and classism reach
and their effect on not only the healthcare system but, the other systems that coincide
with how our medical model operates. This is a large-scale problem that has so many
controversial opinions on how to solve it but, the addition of community healthcare
workers into this pipeline eases the process of finding resources that accommodate
specific situations. Hassan’s role is a multifaceted one that takes on the role of a medical
educator, social advocate, and legal consultant. He encapsulates three very different fields
but is able to combine them into a role that specializes in providing equal access. This
type of role is the very antithesis for what the general Western healthcare provider looks
like. Rather than conforming to a homogenous-centric model of care, community
healthcare workers are responsible for zeroing in on the different communities that they
serve.
In being that healthcare advocate, Hassan’s job also focuses on essentially utilizing
whatever tools he can to bypass systemic barriers. These previously mentioned barriers
come from the existing prejudice not only in medicine but in all aspects of society. In
Kristin Langellier’s chapter of Applied Communication in Organizational and
International Contexts, the author discusses how when the Somali Bantus arrived in
Maine, Lewiston mayor Laurier T. Raymond wrote an open letter to Somali community
advocates and leaders asking for the discouragement of future arrivals. Following this, a
34

white supremist group called the World Church of the Creator held a rally in Lewiston,
declaring through anti-immigration sentiments that they were there to “save” the city. It is
with this that I argue, how could the medical system truly be impartial when our
government leaders are encouraging the exclusion of marginalized communities from
seeking safety in our country? These are the problems that community healthcare workers
such as Hassan seek to address through his advocacy work.
After having the opportunity to speak with Hassan, something that became a part
of the two-pronged hypotheses approach to my thesis was the idea of supplementing
existing medical providers with healthcare workers in the Western model. While this was
a more large-scale recommendation that I formulated after my research, it is certainly
something that I believe to be an important step towards stepping away from the idea that
literacy and access are not connected. They are both intertwined because of hegemonic
values concerning how the system makes it difficult for marginalized communities to find
and access resources while also having no sense of how to navigate the healthcare
system.
In terms of specialized branches of medicine, Hassan brought up an interesting
point about natal care for the Somali Bantu community, which was something that came
up in my preliminary analysis of literature. He discussed how there were certain
exceptions to the staunch criteria of regional healthcare for expectant mothers. There
were three main secondary sources for this thesis that looked at overall healthcare
experiences in a clinical setting for Somali women. One was a general overview of the
35

experience of Somali women in a clinical setting and the other two were more specific to
pre and post-natal care. The first publication was a qualitative study that took place in
Rochester, NY and looked at the provider-patient relationship for 34 Somali women.
While this was a study conducted in New York, it pointed to similar themes that were
found in other colleague’s publications about Somali women’s healthcare experiences in
Maine. In terms of access to emergency medical services, which often is the only one that
Somali women qualify for, one patient stated: [If I don’t] have transportation I can’t go to
the hospital. That’s the problem. And if I don’t have anybody to make the appointment
for me I can’t do it [myself]. Translators are needed.” (Carroll 340). This again ties back
to that idea of not having the ability to have access if one’s healthcare literacy is not
supported by existing systems. Another aspect of this study that touched upon the value
of understanding a patient’s identity was the level of comfort patients felt in settings that
were not male-dominated. The study found that 62% of patients were more comfortable
discussing their medical concerns if their provider was female-identifying. This is
touched upon in another piece on dynamics of both expectant and recent Somali mothers.
In a Portland-based journal article on group dynamics of Somali women, settings with
female nurses who had previously worked with the community yielded positive results in
“...[because] they had experience working with Somali women, they were able to develop
trust and comfort in the groups with a relaxed and conversational approach” (Hill et al.
74). This particular study explored the different taboo topics, such as mental health with
natal care, which is so important when talking about healthcare. It is a perfect
representation of how understanding and respecting your patient’s identity can make a
36

clinical visit run more effectively for both parties. The third piece on Somali women’s
health was a journal article from the Journal of Midwifery and Women’s Health where
they discussed health literacy for a group of Lewiston-based Somali Bantu women. “The
authors found limited health literacy in a population of immigrant Somali women and
created historietas (comic-book style health education brochure) that could be utilized by
health care providers to improve communication and understanding of perinatal health,
including emergency cesareans and postpartum depression…”(Jacoby et al. 594). What
this article brings into the argument is another example of health literacy being limited
because of communication issues. These expectant mothers were not able to effectively
communicate their inquiries to providers because of a language barrier and a difference in
cultural understanding surrounding medicine. However, this is an issue that is directly
linked to how the medical model works.
Another important piece of the argument concerning health literacy that Hassan
provided more context to was the idea of language interpretation. According to Hassan,
most health providers do not speak Somali and are white-identifying. However, large
regional medical institutions, such as MaineHealth are attempting to bring in more
interpreters that can effectively aid in provider-patient interactions. Examples of how
non-for-profits are partnering with large health partners to create more translated
resources can be seen in Appendix B. Figures 3 and 4 refer to COVID-19 vaccine
information and safety protocols about how to respond if one were to come into close
37

contact with an individual who tested positive. It also gives helpful background on the
vaccines and where it is possible to get it administered around the state of Maine.
Figure 5 is an infographic that details the COVID-19 Vaccine Initiative within the
City of Portland Public Health’s Minority Health Program. The latter was founded to
include marginalized voices in the conversation about the COVID-19 pandemic and how
to provide access to prevention resources, as well as provide more information regarding
the available vaccines. These flyers were distributed to the greater Southern Maine area
where there is the highest concentrated population of Somali Bantus. There is a push
from those that have been advocating for the community for years to incorporate
technology such as language translation and interpretation. And, as Hassan stated, this
change is starting to happen. There is a need for even more providers that can speak
Somali or have an assistant interpreter because it is a human right to receive medical care
that is equitable in all sense of their identity.
This technology solution to the societal problem surrounding science is one that,
after conversing with Hassan, began to take shape as a possible response to my second
initial hypothesis regarding how access and literacy are directly linked to large governing
bodies. It becomes more clear that it is less about the fault of the communities on whether
or not they actively seek out medical resources but, it is a reflection of institutions
shifting the burden onto them.
38

In connecting with Hassan and MAIN, I was not only able to get more insight into
how the healthcare system of Maine disadvantages the Somali Bantu community but, it
gave me even more context into the Western model of medicine.
A Field Analysis of the Somali Bantu Community Association
The Somali Bantu identity is a unique and complex one that the Somali Bantu
Community Association (SBCA) was founded to both celebrate and give the New
Mainers an outlet in which they could have full autonomy over the food they grow to
sustain and nourish their bodies. Farming, as Libah describes, is a pinnacle in the Somali
Bantu identity. Before they arrived in the United States, farming was essentially “life”. In
their home country, agriculture was the main source of sustainability for the Somali
Bantus. His response to the provided prompts was a combination of how medical
reconciliation with their agricultural identity has blossomed into an organization that
values community empowerment as a cornerstone of a holistic medical system. The
SBCA reclaims their narrative through land cultivation. When they faced discrimination
on a structural and military level, they were stripped of their ancestral lands. It was on
these lands that they grew crops, which nourished them and provided them a space for
community healing. After this was taken from them, they arrived in Maine where they
were met with further systemic violence. After the Somali Bantus arrived in Maine, they
faced both a lack of food and security. Those who qualified relied on food stamps and
39

community pantries to sustain their families. In terms of land ownership, there were often
retracted leasing offers that reflected the somewhat hostile response to their arrival. A
Yarmouth resident noted that, “Cultural differences, misunderstandings and
miscommunications” had sometimes prompted landlords to terminate the lease” (Lim 2).
However, regardless of intention, the Somali Bantu community was isolated from the
domestic community. However, Muhidin Libah had a vision that they would succeed in
their vision to gain land and rebuild their farming community. He founded Little Jubba
farms and the SBCA, which finally found stretches of agrarian green to begin their
cultivation of staple crops just in time for the spring bloom.
Their interesting contribution to the healthcare narrative about access is one that
truly builds from the ground up. The biggest access barriers to sustainable agricultural
health is a lack of land ownership. Recounting the emotion of being able to plant the first
seeds in the Maine soil following the SBCA’s founding, members reflected back on their
roots as farmers who lived and healed off the land. The impact of having the ability to
farm in Maine was enormous because it meant that the Somali Bantus would be able to
have a stake in their own health. Their story is one that speaks volumes about having
autonomy over one’s own health. In clinical settings where they are unfamiliar with
certain practices and procedures, having the ability to feed their body with food that they
have grown is a step towards medical reconciliation between the West and other cultures.
The SBCA’s narrative is very similar to the small seeds that they plant into the ground; it
grows long branches that stretch far into the soil around it. In creating a space where
40

health and wellness meet, future generations will be positively affected by the advocacy
done by those that came before them with a simple dream.
In addition to bridging access gaps with agricultural wellness, SBCA also provides
many different resources for preemptive health education. They address nutrition,
exercise, managing diabetes, information about prescription medications, and insurance
coverage through their medical reconciliation program. Their approach in combining
traditional Somali healing techniques and Western diagnoses is an interesting model that,
after my research, would be a fascinating potential medical education compromise.
Anew, there is an aspect of my research that directly correlates with the thesis’ two main
hypotheses. By interpreting health literacy through their own lens, the SBCA garners
health access by distributing their own healthcare narratives to better advocate for a more
inclusive system. They also take the burden that has been shifted onto them by the system
and create their own well of resources that can be accessed by Somali Bantus across
Maine and serve as that aforementioned holistic model to medical providers.
All in all, Muhidin Libah’s testament about his own creation was not only
enlightening but gave this thesis more depth in terms of the spectrum that healthcare
alternatives can have. The SBCA’s approach certainly echoed the points made by
MAIN’s push for more specialized healthcare workers and the importance of
incorporating identity into how health is viewed.
41

Conclusion
Intertwining scholarly literature and my own field work, my thesis was meant to
act as supplemental structuring for the Southern Somali community’s healthcare
narratives. In terms of my findings, it is clear that the established health literacy dilemma
stems from prejudicial structures within medicine. However, the problem does not simply
start and end with how providers are taught. It involves how marginalized communities,
such as the Somali Bantu communities are viewed in the scheme of health access and
literacy. A bulk of the burden concerning their lack of options is shouldered onto their
community. The organizations that I developed ties with are both instrumental to not only
addressing the systemic issues but provide their own identity-based solutions. The reality
is that because they are disadvantaged in the mainstream system, they are at risk for
developing health issues that are not properly treated. Within the Somali Bantu
community, some of the biggest health concerns were “health behaviors (22.7%),
diabetes (18.2%), and hypertension (14.4%), while those of the community were diabetes
(22.5%), hypertension (18.8%) and weight (15.9%)” (Mohamed et al. 458). These
conditions are all treatable, however, the lack of clarity from the health industry make it
difficult for this New Mainers generation to have a strong support system. The existing
barriers are due to medical school education failing to understand intersectional identities,
not following a community health worker- centered model for newly established
communities, and failing to acknowledge a medical reconciliation model that favors
cultural humility. Provided historical context, the Somali Bantus have been discriminated
42

against in their own country and experienced the same type of sentiments in the United
States. The contemporary Western healthcare model is complex and faceless. However, I
believe that it is possible to refrain from placing blame and giving the burden of
healthcare navigation. It is possible to embrace identity through healthcare and utilize
healthcare workers and agricultural advocates to ensure a more equitable future. To be
privy to the community narratives and have the ability to garner insight from community
organizations was extremely humbling. This thesis is an extension of the passion I have
for bettering healthcare and giving different communities the platform they deserve to
ensure a better tomorrow for their future generations.
43

Bibliography
1. Agrawal, Pooja, and Arjun Krishna Venkatesh. “Refugee Resettlement Patterns
and State-Level Health Care Insurance Access in the United States.” American
journal of public health vol. 106,4 (2016): 662-3. doi:10.2105/AJPH.2015.303017
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4816078/
2. Anderson, Cynthia, Home Now: How 6,000 Refugees Transformed an American
Town (New York: Public Affairs, 2019).
3. Anderson, Warwick. “Teaching `Race' at Medical School.” Social Studies of
Science, vol. 38, no. 5, 2008, pp. 785–800.,
https://doi.org/10.1177/0306312708090798.
https://journals.sagepub.com/doi/pdf/10.1177/0306312708090798
4. Bell, Susan E. "Interpreter assemblages: Caring for immigrant and refugee patients
in US hospitals." Social Science & Medicine. 226 (2019): 29-36.
doi:10.1016/j.socscimed.2019.02.031. Epub 2019 Feb 26. PMID: 30831557.
https://pubmed.ncbi.nlm.nih.gov/30831557/
5. Besteman, Catherine, Making Refuge: Somali Bantu Refugees and Lewiston,
Maine (Durham: Duke University Press, 2016)
44

6. Caldwell, Josh; Metsch-Ampel, Dylan; and Moise, Isa, "Addressing Barriers for
New Mainers in Understanding and Utilizing Transportation Resources to Access
Medical Care and Finding Culturally Appropriate Solutions for the Barriers" .
Community Engaged Research Reports (2018). 60.
https://scarab.bates.edu/community_engaged_research/60
7. Carroll, Jennifer et al. “Caring for Somali women: implications for
clinician-patient communication.” Patient education and counseling vol. 66,3
(2007): 337-45. doi:10.1016/j.pec.2007.01.008
8. Cowenhoven, Julia Lane. "Educating Providers on the Value of Community Health
Outreach Workers in the New Mainer Population." University of Vermont Larner
College of Medicine. (2017).
https://scholarworks.uvm.edu/cgi/viewcontent.cgi?article=1291&context=fmclerk
9. Fitzgerald, Hayley. “Barriers to mental health treatment for refugees in Maine: an
exploratory study.” Journal of Public Health Issues and Practices (2017).
https://scholarworks.smith.edu/cgi/viewcontent.cgi?article=2969&context=theses
45

10. Hakim, Matteen, "Identifying Barriers to Healthcare Access for the Somali
Population at CMMC" (2016). Family Medicine Clerkship Student Projects.
11. Hassan, Mohammed. "Re: Hello from Colby College: Honors Thesis." Received
by Jordan McClintock, April 6, 2022.
12. Hill, Nancy, Emmy Hunt, and Kristiina Hyrkäs. “Somali Immigrant Women’s
Health Care Experiences and Beliefs Regarding Pregnancy and Birth in the United
States.” Journal of Transcultural Nursing. 23, no. 1 (January 2012): 72–81.
https://doi.org/10.1177/1043659611423828.
13. Houston, Ashley R., et al. “You Have to Pay to Live: Somali Young Adult
Experiences With the U.S. HealthCare System.” Qualitative Health Research, vol.
31, no. 10, Aug. 2021, pp. 1875–1889, doi:10.1177/10497323211010159.
14. Huisman, Kimberly A. Editor; Hough, Mazie Editor; Langellier, Kristin M. Editor;
and Nordstrom Toner, Carol Editor, "Somalis in Maine: Crossing Cultural
Currents" (2011). Faculty and Staff Monograph Publications. 48.
https://digitalcommons.library.umaine.edu/fac_monographs/48
46

15. Iftin, Abdi Nor, Call Me American (New York: Knopf Doubleday Publishing
Group, 2015)
16. Ineza, Darlene et al. “Barriers to Healthcare Access for New Mainers.” CORE.
(2019).
https://www.bowdoin.edu/news/2018/pdf/major-barriers-to-healthcare-access-for-
new-mainers-2-1.pdf
17. Jacoby, Susan D et al. “A Mixed-Methods Study of Immigrant Somali Women's
Health Literacy and Perinatal Experiences in Maine.” Journal of midwifery &
women's health vol. 60,5 (2015): 593-603. doi:10.1111/jmwh.12332
18. Khan, Shamaila. “Cultural Humility vs. Competence - and Why Providers Need
Both.” HealthCity, Boston Medical Center, 9 Mar. 2021,
https://healthcity.bmc.org/policy-and-industry/cultural-humility-vs-cultural-compe
tence-providers-need-both.
47

19. Langellier , Kristin M. “ICC 2006: 20th International Colloquium on
Communication - Applied Communication in Organizational and International
Contexts - Table of Contents.” Virginia Tech Scholarly Communication University
Libraries, Digital Library and Archives of the Virginia Tech University Libraries,
2006, https://scholar.lib.vt.edu/ejournals/ICC/2006/.
20. Libah, Muhidin. “Re: Hello From Colby College: Honors Thesis.” Received by
Jordan McClintock. April 4, 2022.
21. Liebman, A. et al. “Agricultural Health and Safety: Incorporating the Worker
Perspective”, Journal of Agromedicine, 15:3, 192-199, (2010), doi:
10.1080/1059924X.2010.486333
22. Lim, Audrea. ““We’re trying to re-create the lives we had”: the Somali migrants
who became Maine farmers”. The Guardian, 25 Feb 2021.
https://www.theguardian.com/environment/2021/feb/25/somali-farmers-maine
23. Maine Access Immigrant Network. “About Us.” MAIN,
https://main1.org/about.php.
48

24. Mohamed, Ahmed A et al. “An Assessment of Health Priorities Among a
Community Sample of Somali Adults.” Journal of immigrant and minority health
vol. 24,2 (2022): 455-460. doi:10.1007/s10903-021-01166-y
25. Nelson, Alondra. Body and Soul: The Black Panther Party and the Fight against
Medical Discrimination. (Minneapolis: University of Minnesota Press 2013).
Print.
26. “Somali Bantu Community Association (SBCA).” Somali Bantu Community
Association, 2022. https://somalibantumaine.org/
27. Spitzer D L et al. “Towards inclusive migrant healthcare.” BMJ; 366 :l4256
(2019). doi:10.1136/bmj.l4256
https://www.bmj.com/content/366/bmj.l4256.abstract
28. Sun, Nina et al. “Human Rights and Digital Health Technologies.” Health and
human rights vol. 22,2 (2020): 21-32.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7762914/
49

29. Xin, Huaibo. "A Review of Refugees’ Access to Health Insurance in the USA."
Journal of Public Health Issues and Practices. 2018, 2: 119
https://doi.org/10.33790/jphip1100119
30. United States Department of Agriculture. “Farm Labor.” USDA ERS - Farm
Labor, 15 Mar. 2022, https://www.ers.usda.gov/topics/farm-economy/farm-labor/.
50

Appendix A: Outreach Materials
Consent for Participation in Interview
I volunteer to participate in a research project for an honors thesis conducted by Jordan
McClintock from Colby College in the STS Department.
1. My participation in this project is voluntary. I have the freedom to exit the interview at
any time.
2. If I wish to remain completely anonymous: names, locations, and other details will be
changed to protect anonymity.
→ There will be no other person present in the interview apart from the
interviewer
→ Notes taken by the interviewer will never be shared
3. Participation will be approximately 45 minutes over Zoom or a phone call.
4. I understand that this research study has been reviewed and approved by the
Institutional Review Board (IRB) at Colby College.
51

5. I have read and understand the explanation provided to me. I have had all my questions
answered to my satisfaction, and I voluntarily agree to participate in this study.
Example Interview Questions
Non-for-profit organizations and advocacy groups
● Explain a little about what your organization does to support the Somali
community.
● What is the experience of a newly-arrived family or individual in terms of
obtaining physicals/general health check-ups?
● How have the communities of Southern Maine transitioned after the arrival of the
Somali community?
Healthcare Providers
● What does representation look like in terms of care providers that speak Somali?
● Describe the differences in obtaining clinical care within the Somali community
between someone with documentation and someone without.
● In your opinion, what type of sensitivity training (or anti-bias training) were you
given, if any, during your medical education or residency training.
Somali Community Representatives
52

● How easy it is to receive healthcare (ie: a doctor’s visit, walk-in, etc?)
● Difference in receiving care for documented vs. undocumented.
● Were healthcare resources explicitly outlined upon arrival to the US?
● Is there a discrepancy in healthcare for children- particularly displaced children
that have a sponsor but no legal guardian available?
53

Appendix B: Somali Healthcare Infographics
Figure 3. This Somali-translated infographic details COVID-19 safety protocols and vaccine resources.
https://www.portlandmaine.gov/DocumentCenter/View/30854/Image-COVID-19-Vaccine-60-Flyer-Somali
54

Figure 4. This infographic is a Somali-translated “Do’s and Don’ts” for those who have close contact with someone,
who has tested positive for COVID-19.
https://www.maine.gov/doe/sites/maine.gov.doe/files/inline-files/ENGLISH%20Dos%20and%20Donts%20Flyer.pn
g
55

Figure 5. This Somali-translated infographic is part of the the City of Portland Public Health Division’s Minority
Health Program regarding their COVID-19 vaccine initiative and key contacts.
https://www.portlandmaine.gov/DocumentCenter/View/31758/Vaccine-CHOW-Flyer-Somali?bidId=
56
