
Audit Report
The Social Security
Administration’s Expansion of
Health Information Technology to
Obtain and Analyze Medical
Records for Disability Claims
A-01-18-50342 | January 2022
MEMORANDUM
Date: January 3, 2022
Refer To: A-01-18-50342
To:
Kilolo Kijakazi
Acting Commissioner
From:
Gail S. Ennis,
Inspector General
Subject:
The Social Security Administration’s Expansion of Health Information Technology to Obtain and
Analyze Medical Records for Disability Claims
The attached final report presents the results of the Office of Audit’s review. The objective was
to assess the Social Security Administration’s efforts to expand the use of health information
technology to obtain and analyze medical records for disability claims.
If you wish to discuss the final report, please contact Michelle L. Anderson,
Assistant Inspector General for Audit.
cc: Trae Sommer
Attachment

The Social Security Administration’s Expansion of
Health Information Technology to Obtain and Analyze
Medical Records for Disability Claims
A-01-18-50342
January 2022 Office of Audit Report Summary
Objective
To assess the Social Security
Administration’s (SSA) efforts to
expand the use of health information
technology (health IT) to obtain and
analyze medical records for disability
claims.
Background
To make disability determinations,
SSA (a) manually requests medical
records and receives them in paper
format (mail or fax) or through
Electronic Records Express (ERE),
which is SSA’s secure web portal, or
(b) requests and receives them
automatically from health IT.
Health IT is a broad concept that uses
an array of technologies, such as
electronic health records and
exchange networks, to record, store,
protect, retrieve, send, and receive
medical records securely over the
Internet.
It can take SSA days, week, or months
to obtain paper records. SSA does not
track the time from when it requests
and receives ERE records; whereas
health IT records arrive in seconds or
minutes.
SSA uses its Medical Evidence
Gathering and Analysis through Health
Information Technology (MEGAHIT)
software to automatically request and
receive health IT records and perform
data analysis.
Conclusion
Despite spending more than 10 years trying to increase the
number of medical records received through health IT, SSA still
receives most records in paper or ERE format. In the Fiscal
Year (FY) that ended on September 30, 2020, SSA received only
11 percent of medical records through health IT.
SSA experienced a decreasing trend in adding new health IT
partners from 56 in FY 2018 to 12 in FY 2021 (as of August).
During this time, SSA reduced the number of staff and contractors
involved in health IT outreach and did not fully fund projects to
increase electronic medical evidence. Also, expanding the number
of health IT records by adding new partners is not a unilateral
decision made by SSA, as prospective partners must be willing
and able to meet SSA’s technical requirements, and COVID-19
was a factor. In October 2021, SSA informed us it was (a) working
on Memorandums of Understanding with 3 entities to exchange
health IT records with over 30 large health IT organizations and
(b) adding more staff to develop and implement strategies to
expand health IT.
Challenges in expanding the number of health IT records include
some partners’ inability to send sensitive medical records,
acceptance of SSA’s authorization form to release records to the
Agency (Form SSA-827), and medical industry-wide differences in
patient-identifying data fields.
Additionally, SSA has had limited success analyzing medical
records because MEGAHIT is limited to analyzing only structured
data. MEGAHIT generated data extracts on only 7.3 percent of the
1.6 million health IT records SSA received in FY 2020. The
extracts assist SSA disability examiners in making accurate
disability determinations. Since 2018, SSA has been developing
and testing the Intelligent Medical-Language Analysis GENeration
application with new capabilities for reviewing medical records. As
of August 2021, SSA was still testing and rolling out this application
to its offices.
Recommendation
We recommend SSA intensify efforts to increase the number of
health IT partners. SSA agreed with the recommendation.
SSA’s Expansion of Health IT (A-01-18-50342)
TABLE OF CONTENTS
Objective ............................................................................................................................... 1
Background .......................................................................................................................... 1
The Social Security Administration’s Process for Obtaining Medical Records ............ 2
Benefits of Health Information Technology.................................................................. 4
Prior Report on Health Information Technology ......................................................... 5
Scope and Methodology ................................................................................................. 5
Results of Review ................................................................................................................ 5
The Agency’s Evolving Strategy for Obtaining and Analyzing Medical Records ......... 6
Challenges the Agency Faces in Obtaining and Analyzing Health Information
Technology Medical Records ......................................................................................... 8
Challenges with Obtaining Sensitive Records ........................................................ 11
Challenges with the Agency’s Authorization Form to Obtain Health Information
Technology Records ................................................................................................ 11
Challenges Matching Patient-identification Information ......................................12
Challenges in Analyzing Medical Evidence Electronically ..................................... 13
The Agency’s Plan for Increasing Electronic Medical Records for Fiscal Year 2021
and Beyond ...................................................................................................................14
Recommendation ...............................................................................................................14
Agency Comments .............................................................................................................. 15
– The Social Security Administration’s Medical Record Payment Rates .... A-1
– Prior Report Recommendation Status ...................................................... B-1
– Scope and Methodology ............................................................................ C-1
– Timeline of the Social Security Administration’s Use of Health
Information Technology .............................................................................. D-1
–Summary of Federal Health Information Technology Legislation ........... E-1
– Agency Comments ..................................................................................... F-1

SSA’s Expansion of Health IT (A-01-18-50342)
ABBREVIATIONS
C.F.R. Code of Federal Regulations
DDS Disability Determination Services
ERE Electronic Records Express
Form SSA-827 Authorization to Disclose Information to the Social Security Administration
FY Fiscal Year
GAO Government Accountability Office
Health IT Health Information Technology
HHS-ONC The Department of Health and Human Services, Office of the National
Coordinator for Health Information Technology
IMAGEN Intelligent Medical-language Analysis GENeration
MEGAHIT Medical Evidence Gathering and Analysis through Health Information
Technology
OIG Office of the Inspector General
POMS Program Operations Manual System
Pub. L. No. Public Law Number
SSA Social Security Administration
Stat. Statutes at Large
U.S.C. United States Code

SSA’s Expansion of Health IT (A-01-18-50342) 1
OBJECTIVE
Our objective was to assess the Social Security Administration’s (SSA) efforts to expand the
use of health information technology (health IT)
1
to obtain and analyze medical records for
disability claims.
BACKGROUND
SSA provides Disability Insurance benefits
and Supplemental Security Income disability
payments to eligible individuals.
2
The SSA field office generally forwards the claim to the
disability determination services (DDS) in the State or other office with jurisdiction to determine
whether an applicant is disabled under SSA’s criteria.
3
Disability applicants must inform SSA
about or submit all evidence known to him/her that relates to whether he/she is blind or
disabled.
4
An applicant or his/her representative can submit records directly to SSA. An
applicant can also sign a Form SSA-827, Authorization to Disclose Information to the Social
Security Administration,
5
to allow SSA to obtain copies of medical records from health care
providers that have evaluated, examined, or treated him/her. SSA’s policy states, “Before we
make a determination that the claimant is not disabled, we will . . . [m]ake every reasonable
effort to develop the claimant’s complete medical history.”
6
There are approximately 624,000 physicians and 6,000 hospitals in the United States.
7
In the
Fiscal Year (FY) ended September 30, 2019, health care organizations provided approximately
80.7 percent of the records SSA used to make disability determinations (see Table 1).
1
SSA uses health IT to automatically request and receive disability applicants’ medical information electronically.
2
42 U.S.C. §§ 423 and 1381a.
3
42 U.S.C. §§ 421 and 1383b(a); 20 C.F.R. §§ 404.1601 and 416.1001.
4
20 C.F.R. § 404.1512(a)(1) and 416.912(a)(1).
5
Form SSA-827 serves as a claimant’s written request to release information. SSA, POMS, DI 11005.055,
(October 9, 2014).
6
SSA, POMS, DI 22505.001, B.2 (September 17, 2020). SSA will request medical records and follow-up between
10 and 20 calendar days if it does not receive them. 20 C.F.R. § 404.1512(b)(1) and 416.912(b)(1). See also
42 U.S.C. §§ 423(d)(5)(B) and 1382c(a)(3)(H)(i).
7
Department of Health and Human Services, The Number of Practicing Primary Care Physicians in the United
States, Agency for Healthcare Research and Quality, ahrq.gov (July 2018) and American Hospital Association, Fast
Facts on U.S. Hospitals, 2021 Edition, aha.org (January 2021).

SSA’s Expansion of Health IT (A-01-18-50342) 2
Table 1: Sources of SSA Medical Records - FYs 2017 Through 2019
Source of Medical Records
FY 2017
Number and Percent
of Medical Records
FY 2018
Number and Percent
of Medical Records
FY 2019
Number and Percent
of Medical Records
Health Care Organization,
such as Hospitals and
Physicians
16,832,126 77.5% 16,496,321 78.3% 14,084,934 80.7%
Claimant Representative
8
2,299,553
10.6%
2,156,029
10.2%
1,403,692
8.1%
Consultative Examination
9
2,271,736
10.4%
2,092,081
10.0%
1,757,895
10.1%
Claimant
277,467
1.3%
276,571
1.3%
163,070
0.9%
Educational Facilities
10
50,881
0.2%
49,066
0.2%
42,421
0.2%
TOTAL
21,731,763
100%
21,070,068
100%
17,452,012
100%
The Social Security Administration’s Process for
Obtaining Medical Records
SSA pays approximately $500 million per year to obtain medical records by paper, Electronic
Records Express (ERE), and health IT.
11
Paper consists of medical records SSA obtains through regular mail or fax (or if dropped off
at an SSA office by a claimant or claimant representative.)
12
Paper records can take days,
weeks, or months for SSA to receive because manual processes are involved; most of the
time is spent waiting for records to arrive. This time involves:
o SSA calling, mailing, and/or faxing requests for records with a Form SSA-827;
13
o health care providers receiving requests, pulling records, and sending records to SSA;
o SSA scanning responses that are stored as unstructured data;
14
and
8
Individuals filing an application for Old-Age, Survivors and Disability Insurance benefits or Supplemental Security
Income payments may appoint qualified individuals as representatives to act on their behalf in matters before SSA.
20 C.F.R. §§ 404.1705 and 416.1505, and SSA, POMS, GN 03910.020 (May 1, 2013).
9
SSA authorizes DDSs to purchase consultative examinations including medical examinations, X-rays, and
laboratory tests, when the existing records are insufficient to make a determination. POMS, DI 39545.120, A. (June
5, 2017).
10
Educational facility (such as school) records may contain medical information. SSA, POMS, DI 81020.040, B.3 (d)
(February 11, 2019).
11
SSA, Operations Analysis: Electronic Evidence Acquisition, p. 3 (April 2020).
12
If SSA employees receive medical evidence via email, Agency policy requires they inform the sender that email is
not secure and advise them to mail or fax copies of the records or use the ERE Website. SSA, POMS, DI 81020.060,
B. (June 7, 2011).
13
SSA, POMS, DI 22505.006, B.2 (March 15, 2017). For telephone requests, SSA will mail or fax the
Form SSA-827. SSA, POMS, 22505.030, B.1 (b)(1) (April 2, 2021).
14
Unstructured data cannot be easily organized using pre-defined structures. Examples specific to healthcare
include radiology images or text files, like a physician’s notes in the electronic health record. Healthcare Structured
vs. Unstructured Data, https://partners.healthgrades.com/blog/deep-data-dive-structured-and-unstructured-data-in-
healthcare-marketing (May 10, 2021).

SSA’s Expansion of Health IT (A-01-18-50342) 3
o SSA paying for records by individual check (see Appendix A for State payment rates for
medical records obtained via paper or ERE.)
ERE allows organizations to upload records directly into claimants’ unique SSA electronic
folders
15
via SSA’s secure Website using a barcode SSA provides.
16
According to SSA, it
receives ERE medical records faster than paper records because of the electronic exchange
process for receiving the records. However, SSA does not track the time from when it
requests and receives ERE records.
Health IT uses an array of technologies—such as electronic health records and health
information exchange networks
17
—to record, store, protect, retrieve, send, and receive
medical records securely over the Internet. SSA requests and receives health IT records in
seconds or minutes because of the automated process, which involves an SSA system:
identifying health IT partner(s);
sending an electronic request and Form SSA-827 via a health data exchange network;
receiving health IT records as both structured
18
and unstructured data from health IT
partners; and
o electronically paying the federally approved rate of $15 per successful transaction.
In August 2008, SSA partnered with a medical provider to pilot a prototype application called
Medical Evidence Gathering and Analysis through Health Information Technology (MEGAHIT)
and developed standards for the patient-authorized release of health IT records.
19
SSA uses
MEGAHIT to automatically request, receive, and analyze health IT records from partner
organizations. SSA’s health IT partners consist of healthcare organizations, health information
exchanges, and other Federal agencies. MEGAHIT’s data analytics function uses a set of
business rules based on SSA’s Listing of Impairments.
20
MEGAHIT business rules include
rules for cancers, blindness, amputations, transplants, etc. This functionality analyzes the
medical information by looking at diagnosis codes, treatment codes, and other factors and alerts
the examiner to significant information. For example, MEGAHIT creates an alert, such as
15
SSA’s electronic folder contains a claimants’ disability information. SSA, POMS, DI 81001.005, B
(September 11, 2020).
16
SSA, Use Electronic Records Express to Send Records Related to Disability Claims, Publication 05-10046
(September 2020). Some providers use vendors to release records to SSA via secure file transfers or web services.
17
A health information exchange network allows health care organizations to appropriately access and securely
share patients’ medical information electronically.
18
Structured data can be found in any healthcare database and may include details like customer names and contact
information, lab values, patient demographic data and financial information. Healthcare Structured vs. Unstructured
Data, https://partners.healthgrades.com/blog/deep-data-dive-structured-and-unstructured-data-in-healthcare-
marketing (May 10, 2021).
19
SSA, OIG, Health Information Technology Provided by Beth Israel Deaconess Medical Center and MedVirginia, A-
01-11-11117 (October 2011).
20
SSA’s Listing of Impairments describes, for each of the major body systems, impairments that the Agency
considers to be severe enough to prevent an individual from performing gainful activity, regardless of his or her age,
education, or work experience. 20 CFR §§ 404.1525(a) and 416.925(a). An impairment medically equals a Listing if
it is at least equal in severity and duration to the criteria of any listed impairment. 20 C.F.R. §§ 404.1526(a) and
416.926(a). If a condition meets or medically equals a Listing, and the claimant is not performing substantial gainful
activity, SSA will find the claimant disabled. 20 C.F.R. §§ 404.1520(b) and (d) and 416.920(b) and(d). SSA, POMS,
DI 24508.010 (February 13, 2018); DI 24508.005 (April 2, 2018); and DI 34000.000 (July 22, 2021).

SSA’s Expansion of Health IT (A-01-18-50342) 4
“. . . preliminary computer analysis indicates that ‘specific listing’ should be considered in this
case.” As additional health IT documents are added to the claimant’s electronic folder, the rules
are rerun across both the new and existing health IT documents looking for matches. See
Figure 1 for a flowchart of SSA’s processes to obtain and analyze medical records.
Figure 1: SSA’s Processes to Obtain and Analyze Medical Records
Benefits of Health Information Technology
As shown in Table 2, SSA makes disability determinations quicker with health IT records; and a
faster allowance determination by SSA means disabled beneficiaries have quicker access to
cash benefits and health care coverage. In a prior review, we concluded the wait for benefits
affected at least one aspect of a disability claimant’s life, such as their finances, access to
medical care, and relationships.
21
21
SSA, OIG, Congressional Response Report: Impact of the Social Security Administration's Claims Process on
Disability Beneficiaries, A-01-09-29084 (September 2009).

SSA’s Expansion of Health IT (A-01-18-50342) 5
Table 2: Comparison of Initial Case Processing Times with and Without Health IT
Records for FYs 2017 Through 2020
FY
Average Processing
Time for Cases
Without Health IT
Records (Days)
Average Processing
Time for Cases with at
Least One Health IT
Record (Days)
Average Processing
Time for Cases with
Only Health IT
Records (Days)
2017
89
79
59
2018
91
82
61
2019
95
88
64
2020
107
101
70
Prior Report on Health Information Technology
In a 2015 audit, we found that despite challenges, SSA continued to expand the number of
health IT partners and had 38 health care partners in 30 States and the District of Columbia. In
addition, the DDS reported they were generally satisfied with MEGAHIT; however, some
suggested SSA improve formatting for health IT records to emphasize dates of treatment and
omit retracted or repetitive information. We found that MEGAHIT received health IT records
19 days faster than paper and ERE medical records.
22
We made four recommendations that
SSA agreed with and implemented; see Appendix B.
Scope and Methodology
We reviewed SSA’s processes to obtain medical records; efforts to expand health IT; and use of
data analytics to evaluate medical records. We identified a population of 1.7 million individuals
who had a health IT request in SSA’s electronic folder with a case establishment date in
Calendar Years 2016 through 2018. From this population, we analyzed a random sample of
275 cases. We also interviewed managers and staff at the U.S. Department of Health and
Human Services’ Office of the National Coordinator for Health Information Technology (HHS-
ONC) about the nation-wide expansion of electronic health records. See Appendix C for our
scope and methodology.
RESULTS OF REVIEW
Although SSA has generally met its targets for increasing the use of health IT to obtain medical
records, the Agency still receives most of the medical records it needs to make disability
determinations in paper or ERE format—not as health IT, see Figure 2. (See Appendix D for a
timeline of SSA’s efforts to electronically obtain and analyze medical records.) Since FY 2018,
SSA has experienced a decreasing trend in adding new health IT partners. SSA reduced the
number of staff and contractors involved in adding new health IT partners, and the Agency did
not fully fund projects to increase electronic medical evidence. In addition, prospective partners
must be willing and able to meet SSA’s technical requirements, including an ability to send
sensitive medical records, acceptance of SSA’s authorization form to release records to the
22
SSA, OIG, The Social Security Administration’s Expansion of Health Information Technology, A-01-13-13027, p 10
(May 2015).

SSA’s Expansion of Health IT (A-01-18-50342) 6
Agency (Form SSA-827), as well as medical industry-wide differences in patient-identifying data
fields. In October 2021, SSA informed us it was increasing its efforts by working on
Memorandums of Understanding with three entities to exchange health IT records with over
30 large health IT organizations.
Figure 2: Number and Type of Medical Records - FYs 2016 Through 2020
9,372,392
9,200,753
8,656,254
6,814,388
7,056,697
5,073,931
6,980,627
6,885,301
5,864,376
6,004,051
455,174
650,746
954,766
1,406,170
1,560,916
0
1,000,000
2,000,000
3,000,000
4,000,000
5,000,000
6,000,000
7,000,000
8,000,000
9,000,000
10,000,000
FY 2016 FY 2017
FY 2018 FY 2019 FY 2020
Number of Records
Fiscal Years
Paper ERE Health IT
34%
3%
4%
6%
10%
11%
63%
41%
55%
42%
52%
42%
48%
41%
48%
Addi
tionally, SSA has had limited success in expanding its data analytics of medical records to
assist adjudicators in determining whether claimants are disabled. As of FY 2021, SSA was
exploring options to automatically analyze all medical record formats (paper, ERE, and health
IT).
The Agency’s Evolving Strategy for Obtaining and
Analyzing Medical Records
The Agency’s 2014 Open Government Plan included a major health IT initiative to reduce the
time to obtain medical records needed to support disability determinations and manage the
information more efficiently. Per SSA’s plan, using health IT provides:
a fully automated request and receipt process for medical evidence;
more complete and standards-based medical records; and
faster disability decisions using extensive rules-based decision support.
SSA’s plan was to continue its outreach efforts in FYs 2014 through 2016 to include additional
medical providers and collaborate on setting government-wide health IT policy, and by

SSA’s Expansion of Health IT (A-01-18-50342) 7
participating in advisory panels, workgroups, and task forces to ensure SSA’s unique business
needs were included in national standards and policies.
23
In FY 2010, SSA set a baseline target: to increase the percentage of disability cases evaluated
using health IT.
24
In FY 2014, SSA modified the target: to increase the percent of initial
disability claims processed with health IT medical records. The percent of initial claims with
health IT grew from 3 to 14 percent, see Table 3.
Table 3: Increase the Percent of Initial Claims Processed with Health IT Medical Evidence
FYs 2014 Through FY 2017
25
FY
Target for Initial Claims
with Health IT
Percent of Initial
Claims with Health IT
Target Met
2014
2.5%
3.0%
Yes
2015
6.0%
6.1%
Yes
2016
8.0%
9.6%
Yes
2017
12.0%
14.0%
Yes
In FY 2018, SSA modified its performance target again, by combining health IT with ERE
medical records because it determined the health IT performance measure did not accurately
represent its performance in reference to the rate of electronic evidence received. However,
health IT is a fully automated process from the request and receipt of the medical records;
whereas ERE involves the manual request of the records and receipt is through fax or requires
a manual upload to SSA’s system using a bar code.
SSA met its new target for combined health IT and ERE medical records in FYs 2018
26
and
2019 but not in 2020 (see Table 4).
23
SSA, Open Government Plan 3.0 Plan Milestones and Completion Report (June 2014) and SSA, Annual
Performance Report Fiscal Years 2017 - 2019 (February 2018).
24
SSA, Annual Performance Plan for Fiscal Year 2015, Revised Performance Plan for Fiscal Year 2014 and Annual
Performance Report for Fiscal Year 2013, p. 29 (March 2014).
25
SSA’s Annual Performance Report Fiscal Years 2017 – 2019, p. 44 (February 2018).
26
In June 2018, SSA looked into the feasibility of outsourcing the collection of medical evidence to capable industry
vendors on a nation-wide basis
established a panel to determine which vendors
could meet its needs. However, after this review, SSA leadership preferred to consider other alternatives based on
emerging technologies and advances in patient health and took no procurement action related to this effort. SSA
could not provide us with a cost analysis to support this decision. SSA,

SSA’s Expansion of Health IT (A-01-18-50342) 8
Table 4: Improve the Disability Process by Increasing the Percentage of Medical
Evidence Received from Health IT and ERE
FYs 2018 Through 2020
27
FY
Target for Initial
Claims with
Health IT or ERE
Percent of Initial
Claims with
Health IT
Percent of Initial
Claims with ERE
Percent of Initial
Claims with
Health IT and
ERE
Target
Met
2018
45.0%
6.0%
42.0%
48.0%
Yes
2019
50.0%
10.0%
42.0%
52.0%
Yes
2020
60.0%
11.0%
41.0%
52.0%
No
The actual percent of initial claims with health IT records in FYs 2018 through 2020 (Column 3,
Table 4 – 6, 10, and 11 percent) was less than the FY 2017 level (Column 3, Table 3 –
14 percent). Therefore, SSA’s updated strategy did not help it increase the number of health IT
records it received. According to SSA, several factors impacted its ability to meet its FY 2020
target, such as an increase in faxed (non-electronic medical evidence) submissions by
7.26 percent after 3 consecutive years of decreases and setbacks due to the COVID-19
pandemic (that is., Health IT partners redirecting resources).
In its Annual Performance Report for Fiscal Years 2019-2021, SSA’s key initiative was to
Expand Access to Electronic Medical Evidence and it no longer included a specific target for just
health IT records.
We depend on healthcare providers to provide medical records we need to
determine whether a claimant is disabled. Expanding the use of electronic
medical evidence allows disability adjudicators to easily navigate the record to
identify pertinent information, makes it easier for medical providers to submit
evidence, and provides our agency with additional opportunities to use data
analytics to improve the disability process.
28
Challenges the Agency Faces in Obtaining and Analyzing
Health Information Technology Medical Records
The HHS-ONC reported that, in FY 2017, 80 percent of office-based physicians and 96 percent
of non-Federal acute care hospitals used certified electronic health records.
29
Although medical
providers have electronic health records, they may not be able to send those records to SSA.
27
SSA, Annual Performance Report Fiscal Year 2020, p. 20 (January 2021) and Annual Performance Report, Fiscal
Years 2019-2021, p. 18 (February 2020). SSA’s health IT goal for FY 2020 was established before the COVID-19
pandemic.
28
SSA Annual Performance Report, Fiscal Years 2019-2021, p. 18 (February 2020). SSA’s target for electronic
medical evidence includes both ERE and health IT.
29
Health IT Dashboard, United States Health IT Summary, healthit.gov (December 7, 2020). The HHS-ONC
Certification Program assures that a system meets the technological capability, functionality, and security
requirements adopted by the Department of Health and Human Services. The HHS-ONC tracks the adoption of
electronic health records for non-Federal acute care hospitals and office-based physicians in the United States, which
“. . . . comprise a majority of those providers eligible for the Centers for Medicare & Medicaid Services’ Promoting
Interoperability Program, and are the primary source of health care for many Americans.”

SSA’s Expansion of Health IT (A-01-18-50342) 9
The HHS-ONC reported that, in both 2015 and 2017, “. . . about only 1 in 10 physicians
engaged in all 4 domains of interoperability,” which is the ability to send, receive, find, and
integrate health information received from outside sources and use that information to inform
clinical decision-making.
30
Additionally, the “. . . most frequent reported barrier to electronic
exchange was difficulty exchanging data across different [electronic health records] vendor
platforms.”
31
In February 2009, the President signed the American Recovery and Reinvestment Act of 2009
into law.
32
The Act provided $40 million to SSA for health IT research and activities to facilitate
the adoption of electronic medical records, including the transfer of funds to the Supplemental
Security Income Program to carry out activities under the Social Security Act. SSA used over
$17 million of these funds to form health IT partnerships. However, according to the HHS-
ONC,
33
since the American Recovery and Reinvestment Act funds have been completely
distributed, there are no financial incentives for organizations to offset the cost of implementing
an electronic records process.
34
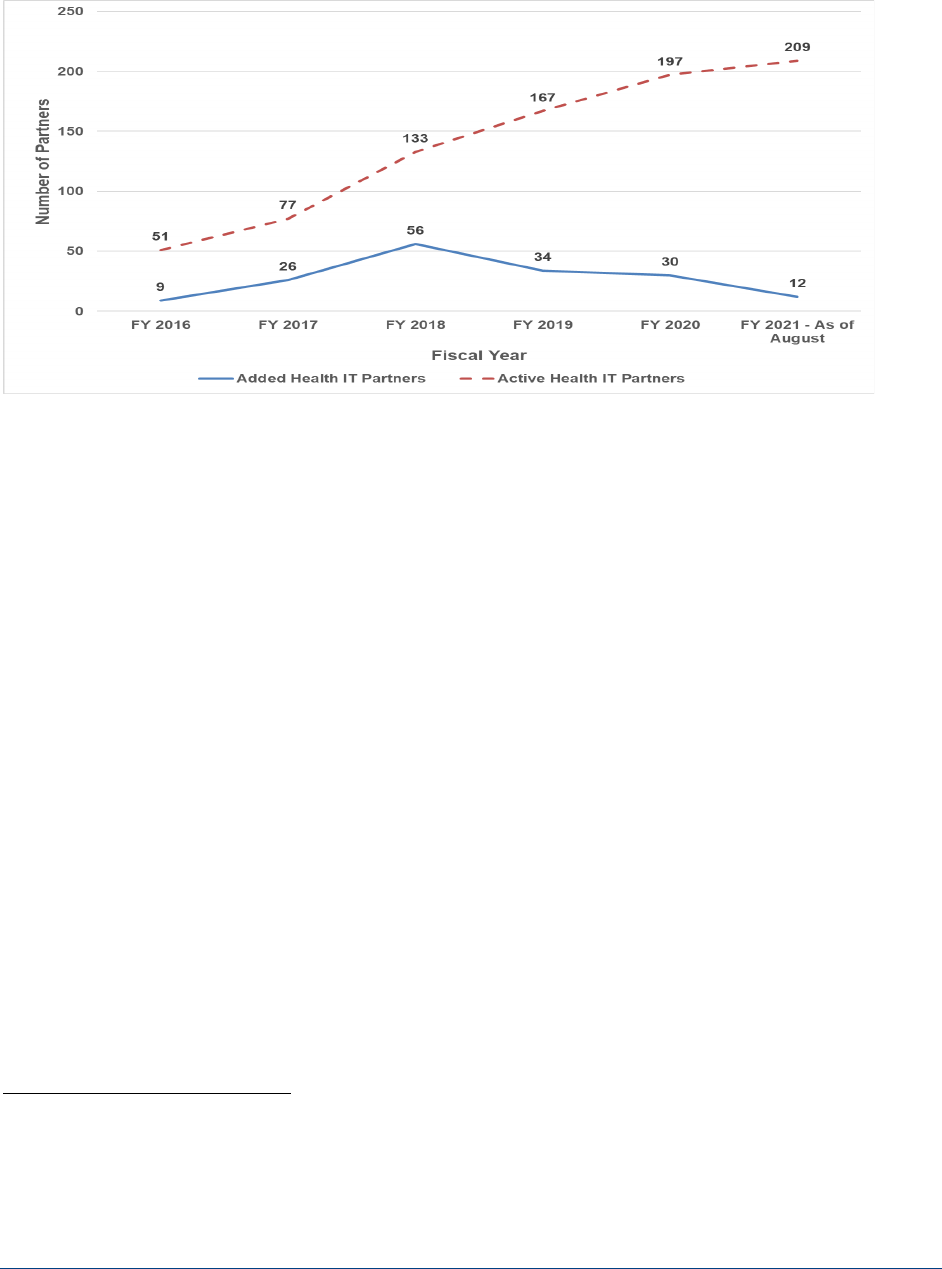
As of August 2021, SSA had added 12 new partners for a total of 209 health IT partners, that
comprised more than 26,000 health care providers in 49 States.
35
However, since FY 2018,
SSA has experienced a downward trend in adding new partners (see Figure 3). SSA informed
us that “There is no way for us to know for certain for FY 2019 [why fewer partners were added].
Adding partners is not a unilateral decision as prospective partners must be willing and able to
partner with us, and each has their own reasons for pursuing or not pursuing this
relationship . . . For FYs 2020 and 2021, we know that the COVID-19 pandemic was the main
factor. Prospective partners reacted to the pandemic and changed their priorities, as with the
rest of the health care industry.”
30
Vaishali Patel, MPH PhD; Yuriy Pylpchuk, PhD; Sonal Parasrampuria, MPH; and Lolita Kachay, MPH,
Interoperability among Office-Based Physicians in 2015 and 2017, The Office of the National Coordinator for Health
Information Technology, ONC Data Brief, No. 47, p. 1 (May 2019).
31
Yuriy Pylpchuk, PhD; Christian Johnson, MPH; Vashali Patel, PHD MPH, State of Interoperability among U.S. Non-
federal Acute Care Hospitals in 2018, The Office of the National Coordinator for Health Information Technology, ONC
Data Brief, No. 51, p. 4 (March 2020).
32
Pub. L. No. 111-5, 123 Stat. 115, 186 (2009).
33
The HHS-ONC—in the Department of Health and Human Services—is the principal Federal entity charged with
coordinating nation-wide efforts to implement and use the most advanced health IT and the electronic exchange of
health information.
34
See Appendix E for a summary of Federal legislation that promotes health IT expansion.
35
SSA does not have health IT partners in Maine. According to SSA, its Health IT Outreach Team contacted
healthcare providers and health information organizations in Maine as far back as 2014. Many of these organizations
have not been able to meet its clinical information requirements or were not interested in sharing electronic health
information with SSA.
SSA’s Expansion of Health IT (A-01-18-50342) 10
Figure 3: Number of Health IT Partners
SSA identifies potential partners from multiple sources including health IT conferences, SSA
regional office staff, DDS referrals, and direct referrals. According to SSA, “Outreach and
relationships are essential to our success. Because we do not have financial incentives, such
as grants, to help healthcare organizations who wish to connect with us, we must build and
maintain relationships with partners, technology vendors, and the DDS.”
36
SSA informed us
that it could onboard approximately 50 partners in an FY, assuming it can get that many to
agree to partner with SSA.
According to SSA, in FY 2021, it had eight staff working on health IT outreach and one subject
matter expert focused on developing strategies to expand health IT. However, around 2018,
when SSA was bringing more partners on board (as seen in Figure 3), it had more staff working
on outreach. Staff used to range from 8 to 10 (4 or 5 full-time employees and 4 or 5
contractors). The most was 12 (8 full-time employees and 4 contractors). In October 2021,
SSA informed us that it was re-starting its efforts to expand health IT and its overall strategy is
to add two more experts. The experts will advise the Agency on further developing health IT
strategies to increase health IT medical records. SSA stated it will continue partnering with
organizations that use Epic
37
software and the eHealth Exchange network, but that it was
developing new strategies for expanding the health IT records beyond this. SSA prioritizes
adding partners who use Epic electronic health record software because Epic provides broad
support for the data elements SSA needs to make disability determinations. According to SSA,
36
SSA, Office of Systems, Systems F.A.C.T.S. – January 2020, Health IT: HITting a Home Run, p. 1 (January 2020).
DDSs are generally State-run agencies that make disability determinations for SSA using the Agency’s regulations,
policies, and procedures; 42 U.S.C. §§ 421 ((a)(2) and 1383b (a).
37
Academic medical centers, community hospitals and other health care providers use Epic electronic health record
software to store patients’ records.

SSA’s Expansion of Health IT (A-01-18-50342) 11
“Epic is … an early adopter of the eHealth Exchange,
38
which creates a natural synergy as it is
the primary network that we use to onboard new organizations.”
Challenges with Obtaining Sensitive Records
Some potential health IT partners restrict sharing health records for anyone under age 18, while
others cannot provide such sensitive records as substance abuse and mental/behavioral
records. According to the HHS-ONC, “. . . because of State or local privacy and security laws,
sensitive records may not be sent through Health IT.” The HHS-ONC has set the minimum
clinical requirement for sharing health information electronically. Many healthcare
organizations, along with their associated electronic health record systems, look to the HHS-
ONC to establish additional standards and specifications to enable electronic sharing of more
types of clinical information electronically. According to the HHS-ONC, the basic requirements
to expand data elements should come online over the next few years.
From our 275-case sample, we identified 13 unsuccessful MEGAHIT requests for sensitive
records. For instance, on August 24, 2018, MEGAHIT requested a Colorado child’s speech
therapy records. The partner’s system responded with “no patient match.” After reviewing
SSA’s electronic records for this claimant, we could not determine why MEGAHIT’s response
was unsuccessful. However, the claimant was 3- years-old when the application was filed. On
October 2, 2018, SSA mailed a follow-up request and received the medical records via paper
(not health IT) on October 5, 2018. Instead of receiving the records via health IT on August 24,
2018 when it initially requested them, it took 42 days for SSA to receive the records.
Challenges with the Agency’s Authorization Form to Obtain
Health Information Technology Records
SSA has also experienced challenges with health record providers not accepting its Form SSA-
827. Some health IT partners:
only accept Form SSA-827s with a wet signature or eAuthorization;
will only release records that are dated before the date the claimant signed the Form SSA-
827;
will not release records if the Form SSA-827 signature is older than 60 days;
require a signature on their own release form in addition to the Form SSA-827; and
may ask for an updated Form SSA-827 signed by someone applying on the claimant’s
behalf.
In November 2019, SSA issued a reminder for staff to review Forms SSA-827 to ensure they
are correctly completed, legible, signed, and dated before transferring the case to the DDS.
39
MEGAHIT will not generate a request if the Form SSA-827 is not in the electronic folder within
38
The eHealth Exchange is the largest healthcare information network in the country and is active in all 50 States.
The eHealth Exchange is a network connecting Federal agencies and non-Federal healthcare organizations so
medical data can be exchanged nationwide to improve patient care and public health (ehealthexchange.org
[May 11, 2021]).
39
SSA, AM-19031 REV (November 20, 2019).

SSA’s Expansion of Health IT (A-01-18-50342) 12
5 hours of the system first searching for it, is restricted, or is expired. If the Form SSA-827
prevents an automated MEGAHIT transaction, the system will generate a health IT response
document alerting staff there is an issue, and the request for health IT will not process.
For our sample, we concluded MEGAHIT was working properly because the system generated
an alert notifying staff of invalid information on the Form SSA-827. For example, we identified
six cases where MEGAHIT generated a health IT response document alerting staff there was an
issue with Form SSA-827. For these six cases, MEGAHIT did not send a request for health IT
medical records because it could not identify a Form SSA-827 in the file (two cases), the health
IT partner (Department of Veteran’s Affairs) only accepts wet signatures (three cases), and the
wet-signature was more than 9-months old (one case). For the case where the wet-signature
was too old, the evidence showed that an SSA employee initiated a user triggered request for
health IT records, but MEGAHIT prevented the request because the Oregon claimant’s
signature on Form SSA-827 was more than 9 months old. SSA obtained an updated Form
SSA-827 and then requested the medical records. To mitigate these Form SSA-827 issues,
SSA plans to develop and implement a tool sometime after FY 2021 to automatically validate
paper Forms SSA-827 and flag those with invalid inputs.
Challenges Matching Patient-identification Information
Another obstacle limiting the expansion of health IT records is differences in patient-identifying
data between SSA and its partners. When SSA requests records, it provides its health IT
partners with the claimant’s name, date of birth, Social Security number, address, and gender.
However, the partner decides how to use the data to identify the claimant in its system. To
avoid disclosing the wrong individual’s health record, partners typically provide electronic
records for only exact data-request matches.
From our sample, we identified 31 MEGAHIT requests that were unsuccessful because of
differences between partner and SSA data. For all cases, SSA needed to follow up with a
manual request to obtain the medical records. For example, on March 24, 2017, MEGAHIT
requested a Kentucky claimant’s records. The health IT partner responded with a “no patient
match” document. On April 24, May 11, and May 26, 2017, SSA followed up by manually
triggering MEGAHIT requests and received the same “no patient match” response. On
May 26, 2017, SSA faxed a request for records. On June 5, 2017—73 days after the initial
MEGAHIT request—SSA received records from the partner. The initial MEGAHIT requests
failed because the individual’s first name in SSA’s system, Jane Lyn, did not match that in the
partner’s system, Janelyn.
SSA has been an active partner with the HHS-ONC in creating and setting national
interoperability standards. In 2018 and 2020, SSA participated in HHS-ONC organized patient
matching working sessions to address the industry-wide issue of differences in patient-
identifying data. According to the HHS-ONC, it and its Federal partners are working on a
Trusted Exchange Framework and Common Agreement, which is mandated by the 21
st
Century
Cures Act.
40
Once finalized, this Framework and Agreement should help enable nationwide
exchange of electronic health information across disparate health information networks, and will
outline a common set of principles, terms, and conditions. HHS-ONC’s goal is to have the
Trusted Exchange Framework and Common Agreement finalized in 2022.
40
21
st
Century Cures Act, Pub. L. No. 114-255, § 4003, 130 Stat. 1033, 1165 (2016).

SSA’s Expansion of Health IT (A-01-18-50342) 13
Challenges in Analyzing Medical Evidence Electronically
A challenge SSA faces in enhancing its data analytics is MEGAHIT’s limitation of analyzing only
structured health IT data. SSA receives both structured and unstructured data from health IT
partners. Per SSA, “. . . the more structured documents (non-image) we receive from partners,
the easier it is to execute our business rules…We encourage our partners to provide as much
structured dat[a] or as many coded documents as possible.”
According to SSA, the number of business rules limits the extracts MEGAHIT can generate.
MEGAHIT generated an extract for 7.3 percent of the approximately 1.6 million health IT
records in FY 2020. In our sample review, MEGAHIT generated a health IT extract for 14 of
275 cases (5 percent). The extracts assist SSA disability examiners in making disability
determinations. While SSA has no technical barriers to adding more business rules, it has not
added new rules since 2020 and does not have plans to do so. Instead, in 2018, SSA began
testing a new application called Intelligent Medical-language Analysis GENeration (IMAGEN),
which would:
enable adjudicators to visualize, search, and more easily identify relevant clinical content in
medical records;
directly correlate clinical information from medical evidence to SSA’s disability impairment
listings; and
improve speed and consistency of medical determinations and decisions.
41
IMAGEN automates the analysis of medical record content, provides decisional support to
disability adjudicators, and will create efficiencies and new knowledge in disability case
processing and determinations by using:
optical character recognition to convert imaged documents into machine-readable text;
natural language processing to convert text into structured data;
machine learning and artificial intelligence to mine and model structured data to provide
intelligent insights based on historical claim outcomes; and
a user-interface to provide advanced search, filtering, alerting, annotation, charting,
explanation, and medical record summarization features.
Whereas MEGAHIT business rules are limited to analyzing structured health IT medical
evidence, SSA is designing IMAGEN to retrieve medical records (both unstructured and
structured) in the disability electronic folder and convert them into machine-readable formats.
As of August 2021, SSA continued to test and roll out IMAGEN at its offices and at State
disability determination services.
41
SSA, Office of Systems, Systems Talks, Connecting Through Conversations, IMAGEN (June 19, 2019).

SSA’s Expansion of Health IT (A-01-18-50342) 14
The Agency’s Plan for Increasing Electronic Medical
Records for Fiscal Year 2021 and Beyond
As part of SSA’s IT planning for FY 2021 and beyond, in April 2020, SSA’s Deputy
Commissioner for the Office of Retirement and Disability Policy submitted a proposal to spend
$60.1 million over 5 years for electronic evidence acquisition. The proposal included plans to
explore and prototype options to automatically exchange all medical record formats—paper,
ERE, and health IT—and retrieve medical records from the most appropriate sources in real
time to reduce manual intervention, additional requests, and duplicate records.
42
SSA expects
this strategy will help it attain its targets of moving away from non-electronic records, decreasing
disability determination times, reducing customers’ burdens at claim filing, and reducing
acquisition costs. While board members of SSA’s Information Technology Investment Process
voted to approve the proposed investment, ongoing planning discussions resulted in an overall
program budget reduction. According to SSA, the project’s budget was cut, and therefore, it has
been scaled back. Depending on SSA’s FY 2022 budget, the project will be restarted or left on
pause.
In October 2021, SSA informed us it was jump-starting its efforts to expand health IT. SSA was
working on Memorandums of Understanding with 3 entities to exchange health IT records with
over 30 large health IT organizations. SSA was also planning to:
analyze geographic variations to identify areas of poor coverage to enable outreach and
onboarding of new sources to increase electronic medical records;
identify large non-electronic providers to try to transition them to providing electronic medical
records;
measure medical source performance (response rates, content quality, etc.) to forecast
growth and inform outreach strategy; and
implement automated notifications based on pre-defined conditions (for example, a decline
in medical source response rate, a decline in medical source volume, etc.;) to actively
engage partners.
Should additional funding become available, SSA plans to evaluate acquiring structured medical
evidence directly from claimants, bypassing the need for lengthy provider onboarding
processes.
RECOMMENDATION
We recommend SSA intensify efforts to increase the number of health IT partners.
42
SSA, Operation Analysis Electronic Evidence Acquisition, (April 2020).

SSA’s Expansion of Health IT (A-01-18-50342)
APPENDICES

SSA’s Expansion of Health IT (A-01-18-50342) A-1
– THE SOCIAL SECURITY ADMINISTRATION’S
MEDICAL RECORD PAYMENT RATES
The Social Security Administration (SSA) will pay a fee for medical records obtained from health
care organizations.
1
For health information technology (health IT) records, SSA pays a $15 flat
rate for each successful transaction. For medical records obtained via paper (mail or fax) or
Electronic Records Express, SSA pays $1 or more based on actual State payment rates.
2
See
Table A–1.
Table A–1: State Payment Rates for Medical Records Obtained via Paper or Electronic
Records Express as of June 2020
State General Payment Rates Medical Records
Alabama
Flat fee of $18.00
Alaska
Average payment of $35.00 with a range $30.00-$50.00
Arizona
Flat fee of $13.15
Arkansas
Flat fee of $15.00
California
Range $14.05 to $21.60 dependent on number of pages. Medical records and narrative
reports from the treating physician or other medical source pay the lesser of: $35.00
(maximum) or billed amount
Colorado
Flat fee of $22.00 (additional $8 payment if received within 5 days of request). $30.00 for a
narrative
Connecticut
Payment of $20, if records received in 30 days or less and no payment for records received
after 30 days
Delaware
Flat fee of $15.00
District of
Columbia
Payment of $25.00, if records received within 20 days; $10.00 if records received after
20 days; and no payment if records received after 60 days
Florida
Flat fee of $14 for all medical evidence. Teacher and speech-language pathologist
questionnaires are a flat rate of $16.00.
Georgia
Payment of $15.00; $10.00 per State of Georgia Health Department’s service time; and
$25.00 for completion of Mental Impairment Questionnaire and Denver Childhood
Questionnaire
Guam
Payment of $35.00; $1.00 for Commonwealth of the Northern Mariana Islands first page and
$.25 page thereafter; and $25 for Samoa
Hawaii
Payment of $15.60 and $31.20 for completion of psychiatric questionnaire
Idaho
$15.00 for records or narrative reports, or up to $15.00 if billed less than that
Illinois
Flat fee of $20.00
Indiana
Payment of $14.00 for copies of medical records; $40 completion of mental questionnaire;
and $25.00 for other questionnaires
Iowa
Payment of $35.00 (or as billed if less than $35.00) and for search fee “no records found”
Kansas
$30.00 per response
Kentucky
Payment up to $15.00
Louisiana
Flat fee of $20.00
Maine
Flat fee of $15.00 (or as billed if less than $15.00)
1
SSA, POMS, DI 11010.545 (February 14, 2017).
2
Vermont will pay $20 for medical records only if records are received within 16 days of request date.

SSA’s Expansion of Health IT (A-01-18-50342) A-2
State General Payment Rates Medical Records
Maryland
Payment of $15.00 for copies of pertinent history, physical, and treatment records; $35.00 for
abstract and physical from treating physician, the physical examination should be within
approximately the last 6 months; and $26.00 for abstract and evaluation (within
approximately last 6 months) from treating licensed health care provider such as
Occupational Therapist, Physical Therapist, Licensed Clinical Social Worker
Massachusetts
Payment of $15.00 for report to physician; $10.00 for report to hospital (additional
$10 payment if received within 15 days of request)
Michigan
Flat fee of $15.00
Minnesota
Payment of $35.00 for all medical or psychological records; $10.00 for chiropractic,
audiology, or physical therapist records; and $0 for school, prison, Veterans Administration,
or other Government agency records
Mississippi
Payment of $14.00; $16.00 for mental health centers; and $31.00 for functional data reports
from mental health centers
Missouri
Payment of $26.06 plus $0.60 per page for paper records plus $24.40 if records maintained
off-site; $26.06 + $0.60 per page or $114.17 maximum, whichever is less, for electronic
records; and $26.06 plus $1.00 per page for Microfilm
Montana
Payment of $10.00 for hospital and schools and $25.00 for doctors, clinics, mental health
centers, private entities (payments limited by state law)
Nebraska
Payment of $20.00 for medical records plus $0.50 per page with specific sources having a
max of $100.00; Howard County Hospital - $100 cap up to 500 pages—anything over
500 pages, State will pay $0.50 per page; and $30.00 maximum for Narrative reports
Nevada
Flat fee of $15.00
New Hampshire
Payment of $1.00 per page up to $15.00 maximum for a copy of existing record and
$16.00 for narrative or completion of forms
New Jersey
Flat fee of $10.00
New Mexico
Flat fee of $18.75, (will pay less if billed less).
New York
Flat fee of $10.00
North Carolina
Flat fee of $15.00
North Dakota
Payment of $20.00 for the first 25 pages, then $0.75 for each additional page for paper
records; and $30 for first 25 pages, then $0.25 for each additional page for electronic records
Ohio
Payment of $15.00 for hospital records and $20.00 for doctor records
Oklahoma
Flat fee of $18.00
Oregon
Payment of $75.00 for full narrative reports more than 2 pages; $35.00 for brief narrative
reports; $18.00 for hospitals, doctors and copy companies, 1-10 pages and $0.25 for pages
11-20 and $0.10 for pages 21 and greater with a total maximum fee of $22.50; and $18.00 if
there is no indication of the number of pages (additional $5 payment if received within 7 days
of request)
Pennsylvania
Flat fee of $29.19
Puerto Rico
Flat fee of $25.00 for all records from non-government entities received within 40 days from
original request date
Rhode Island
Payment of $10.00 (additional $5 payment to hospitals if received within 15 days of request);
and $0 for hospitals at the reconsideration level
3
South Carolina
Flat fee of $20.00
South Dakota
Payment of $11.79 for first 25 pages and $.50 for each additional page to a maximum of
$35.00; and $25 for narrative reports
Tennessee
Payment of $20.00 for medical records and $0 for school records
Texas
Flat fee of $18.00
3
If a claimant disagrees with the initial disability determination, he/she can appeal it. 20 C.F.R. § 404.900(a) and
416.1400(a).

SSA’s Expansion of Health IT (A-01-18-50342) A-3
State General Payment Rates Medical Records
Utah
Payment of $15.00 for copy of records; $28.00 for written summary within 12 days; and
$0 for records received after 60 days and for records from schools or Government agencies
Vermont
A provider cannot charge for a copy of a disability applicant’s medical records. Payment of
$20 expedite fee is paid if the records are sent and the invoice is dated within 16 days of
request date
Virginia
Flat fee of $15.00
Washington
Payment of $22.00 for photocopied records up to 20 pages, $.50 per page beyond 20 pages
and $22 search fee for “no records found”
West Virginia
Flat fee of $11.00
Wisconsin
Flat fee of $26.00
Wyoming
Payment of $15.00 for hospital records; $25 for doctors/clinic and child development centers;
and $0 for public school records

SSA’s Expansion of Health IT (A-01-18-50342) B-1
– PRIOR REPORT RECOMMENDATION STATUS
In our May 2015 report, The Social Security Administration’s Expansion of Health Information
Technology, we concluded that, despite challenges, the Agency continued expanding health
information technology (IT).
1
Table B–1 shows the status of the recommendations.
Table B–1: Prior Audit Recommendation Status
Recommendation Status/Resolution
Continue to solicit, on a regular basis, disability
determination services’ (DDS) user feedback in
Medical Evidence Gathering and Analysis
through Health Information Technology
(MEGAHIT) enhancements
In December 2015, the Social Security Administration
(SSA) implemented a communications plan that collects
and monitors recommendations from the regions/DDS’ via
surveys and a discussion board. SSA will continue
conducting periodic surveys to solicit feedback.
We obtained and reviewed documentation of
11 enhancements SSA made to MEGAHIT software.
Enhance procedures to maintain and update
MEGAHIT partner data, such as addresses.
As of April 2016, SSA was holding monthly meetings with
health IT partners to allow for partner updates as needed.
We obtained and reviewed SSA’s health IT onboarding
flowchart, its communications plan, and the call script
SSA’s employees follow for reaching out and obtaining
information from health IT partners.
Enhance methods to improve the use of
information received via health IT.
As of October 2016, SSA was implementing a process to
obtain recommendations from health IT partners and meet
regularly to discuss enhancements.
1
SSA, OIG, The Social Security Administration’s Expansion of Health Information Technology, A-01-13-13027
(May 2015).

SSA’s Expansion of Health IT (A-01-18-50342) B-2
Recommendation Status/Resolution
Increase health IT partners—taking advantage of
nation-wide Federal efforts led by Health and
Human Services’ Office of the National
Coordinator for Health IT.
SSA coordinates with the Health and Human Services’
Office of the National Coordinator for Health IT (HHS-
ONC). In addition, SSA collaborates with the Departments
of Veterans Affairs and Defense on outreach to potential
new health IT partners. SSA also participates in
public/private workgroups to ensure that its business
needs are considered and incorporated into national
policies and standards; and to gather healthcare
organization contacts to partner with SSA.
We obtained active partner information from SSA’s
internal website and determined what year the partner was
added as a participant in the health IT network. Since our
2015 report, SSA added 171 health IT partners.
We interviewed staff at the HHS ONC and reviewed
information on issues, such as inoperability, with
increasing health IT records.

SSA’s Expansion of Health IT (A-01-18-50342) C-1
– SCOPE AND METHODOLOGY
To accomplish our objective, we:
Reviewed applicable sections of the Social Security Act as well as the Social Security
Administration’s (SSA) regulations, rules, policies, and procedures.
Reviewed prior SSA Office of the Inspector General and Government Accountability Office
reports related to electronic medical records.
Analyzed actions SSA took to implement recommendations from our May 2015 report on
The Social Security Administration’s Expansion of Health Information Technology,
A-01-13-13027.
Reviewed information on SSA’s procedures to obtain medical records and use of data
analytics to evaluate medical records as well as the sources and quantity of medical
records.
Examined SSA’s health information technology (health IT) performance and strategic
targets.
Interviewed employees at the Department of Health and Human Services, Office of the
National Coordinator for Health IT, about the nation-wide expansion of electronic health
records.
Interviewed an SSA subject-matter expert on increasing electronic medical evidence.
Obtained SSA’s payment rates to States for medical records.
Obtained a file of 1,700,177 individuals whose electronic folder indicated SSA requested
health IT records in Calendar Years 2016 through 2018. We randomly sampled 275 cases
1
and:
o analyzed health IT requests on case determinations and case adjudication levels;
determined whether SSA’s Medical Evidence Gathering and Analysis through Health
Information Technology (MEGAHIT) requests were successful;
verified that SSA partners responded to MEGAHIT requests an average of less than
1 day; and
calculated case processing times.
1
To conduct this review, we used a simple random sample statistical approach. This is a standard statistical
approach used for creating a sample from a population completely at random. As a result, each sample item had an
equal chance of being selected throughout the sampling process, and the selection of one item had no impact on the
selection of other items. Therefore, we were guaranteed to choose a sample that represented the population, absent
human biases, and ensured statistically valid conclusions of, and projections to, the entire population under review.
Our sampling approach for this review ensures that our reported projections are statistically sound and defensible.

SSA’s Expansion of Health IT (A-01-18-50342) C-2
We conducted our review between April 2020 and August 2021 in Boston, Massachusetts, and
Arlington and Falls Church, Virginia. We determined the data used for this audit were
sufficiently reliable to meet our audit objectives.
We assessed the significance of internal controls necessary to satisfy our objective. This
included an assessment of the five internal control components, control environment, risk
assessment, control activities, information and communication, and monitoring. In addition, we
reviewed the principles of internal controls associated with our objective. We identified the
following components and principles as significant to the objective.
Component 5: Control Activities
Principle 10: Design Control Activities
Principle 12: Implement Control Activities
Component 5: Monitoring
Principle 16: Perform Monitoring Activities
The primary entity audited was the Office of Health Information Technology under the Deputy
Commissioner/Chief Information Officer, Systems. We conducted this performance audit in
accordance with generally accepted government auditing standards. Those standards require
that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a
reasonable basis for findings and conclusions based on our audit objectives. We believe that
the evidence obtained provides a reasonable basis for our findings and conclusions based on
our audit objectives.

SSA’s Expansion of Health IT (A-01-18-50342) D-1
– TIMELINE OF THE SOCIAL SECURITY
ADMINISTRATION’S USE OF HEALTH
INFORMATION TECHNOLOGY
The Social Security Administration (SSA) began obtaining and analyzing health information
technology (health IT) medical records in 2008. Since then, the Agency has expanded its
efforts to electronically obtain and analyze medical records, see Table D–1.
Table D–1: Timeline of SSA’s Efforts to Electronically Obtain and Analyze Medical
Records
Year(s)
Status
2008
Medical Evidence Gathering and Analysis through Health Information Technology
(MEGAHIT) system implemented to obtain and analyze health IT medical records.
2009
SSA partnered with MedVirginia—a coalition of not-for-profit hospitals and physicians—
to expand the use of health IT to exchange records through the Nationwide Health
Information Network.
2011-2015
SSA added 36 health IT partners (through February 2015).
1
2015
SSA expanded to 38 health IT partner organizations in 30 States and the District of
Columbia and identified ways of enhancing health IT case processing and data
analytics.
2017
From Fiscal Years 2014 through 2017, SSA met its performance target to increase the
percent of initial disability claims processed with health IT medical records.
2018
SSA began developing and testing the Intelligent Medical-Language Analysis
GENeration (IMAGEN) application, which would automate the analysis of medical
record content and provides decisional support to disability adjudicators.
SSA changed its performance target by combining health IT with Electronic Records
Express (ERE) medical records because it no longer believed the health IT
performance measure accurately represented its performance in reference to the rate
of electronic evidence received. (ERE allows organizations to upload records directly
into the claimant’s unique SSA electronic folder via SSA’s secure Website using a
barcode SSA provides.)
2020
SSA’s Office of Retirement and Disability Policy/Office of Disability Policy submitted an
electronic evidence acquisition proposal with a key priority to obtain medical records in
electronic and structured data formats.
2021
SSA leadership is reevaluating the electronic evidence acquisition proposal due to a
budget reduction. SSA expanded to 209 health IT partners in 49 States. SSA has no
plans to create any new targeted business rules to analyze health IT records in
MEGAHIT. SSA continued to test and rollout IMAGEN at its offices.
1
For a list of the health IT partners as of February 2015, see Appendix B in SSA, OIG, The Social Security
Administration’s Expansion of Health Information Technology, A-01-13-13027 (May 2015).

SSA’s Expansion of Health IT (A-01-18-50342) E-1
–SUMMARY OF FEDERAL HEALTH
INFORMATION TECHNOLOGY LEGISLATION
Table E–1
Table E–1: Summary of Federal Health IT Legislation
Legislation Summary
Health Information
Technology for Economic
and Clinical Health Act
of 2009
1
Promoted the adoption and use of health IT and established the
Department of Health and Human Services’ Office of the National
Coordinator for Health IT (HHS-ONC) and other committees in
support of this Act.
American Recovery and
Reinvestment Act of 2009
2
Paid approximately $1 million per contract for organizations to
implement electronic record systems and provided that up to
$40 million to be used by the Social Security Administration for health
IT research and activities to facilitate the adoption of electronic
medical records in disability claims.
Medicare Access and
Children’s Health Insurance
Program Reauthorization
Act of 2015
3
Established the national objective to achieve widespread
interoperability with certified electronic health records and required
the Department of Health and Human Services to measure the extent
to which this objective is being met.
21
st
Century Cures Act
4
Defines interoperability and mandated the HHS-ONC develop or
support a trusted exchange framework for trust policies and practices
and for a common agreement for exchange between health
information networks.
Coronavirus Aid, Relief,
and Economic Security Act
5
In an attempt to improve public health infrastructure, the HHS-ONC
will distribute $2.5 million in CARES Act funding to health information
exchanges to support public health uses of information from health
information exchanges. These networks make it easier for health
care organizations to exchange information, ranging from case
summaries to hospital discharge data.
1
Health Information Technology for Economic and Clinical Health Act, Pub. L. No. 111-5, § 3001 (a), 123 Stat. 115,
230 (2009).
2
American Recovery and Reinvestment Act of 2009, Pub. L. No. 111-5, 123 Stat. 115, 186 (2009).
3
Medicare Access and Children’s Health Insurance Program Reauthorization Act of 2015, Pub. L. No. 114-10,
129 Stat. 87, 139 (2015).
4
21
st
Century Cures Act, Pub. L. No. 114-255, § 4003, 130 Stat. 1033, 1160 (2016).
5
Coronavirus Aid, Relief, and Economic Security Act, Pub. L. No. 116-136, 134 Stat. 281 (2020).

SSA’s Expansion of Health IT (A-01-18-50342) E-2
Legislation Summary
21
st
Century Cures Act:
Interoperability, Information
Blocking, and the Office of
the National Coordinator
Health IT Certification
Program Final Rule
6
HHS-ONC is responsible for the implementation of key provisions in
Title IV of the 21
st
Century Cures Act that are designed to advance
interoperability; support the access, exchange, and use of electronic
health information; and address occurrences of information blocking.
7
6
21
st
Century Cures Act, 85 Fed. Reg. 25642, pp. 25642-25961 (2020).
7
Information blocking is a practice by a health IT developer of certified health IT, health information network, health
information exchange, or health care provider that, except as required by law or specified by the Secretary of Health
and Human Services as a reasonable and necessary activity, is likely to interfere with access, exchange, or use of
electronic health information.

SSA’s Expansion of Health IT (A-01-18-50342) F-1
– AGENCY COMMENTS
SOCIAL SECURITY
MEMORANDUM
Date:
12/27/2021 Refer To: TQA-1
To:
Gail S. Ennis
Inspector General
From:
Scott Frey
Chief of Staff
Subject:
Office of the Inspector General Draft Report - "The Social Security Administration’s Expansion
of Health Information Technology to Obtain and Analyze Medical Records for Disability
Claims" (A-01-18-50342) — INFORMATION
Thank you for the opportunity to review the draft report. We agree with the recommendation.
Please let me know if I can be of further assistance. You may direct staff inquiries to
Trae Sommer at (410) 965-9102.

Mission: The Social Security Office of the Inspector General (OIG) serves the
public through independent oversight of SSA’s programs and operations.
Report: Social Security-related scams and Social Security fraud, waste, abuse,
and mismanagement, at oig.ssa.gov/report
.
Connect: OIG.SSA.GOV
Visit our website to read about our audits, investigations, fraud alerts,
news releases, whistleblower protection information, and more.
Follow us on social media via these external links:
Twitter: @TheSSAOIG
Facebook: OIGSSA
YouTube: TheSSAOIG
Subscribe to email updates on our website.

